Highlights
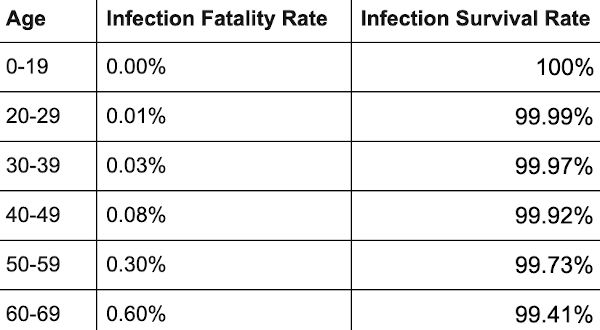
∗ Across 31 systematically identified national seroprevalence studies in the pre-vaccination era, the median infection fatality rate of COVID-19 was estimated to be 0.034% for people aged 0–59 years people and 0.095% for those aged 0–69 years.
∗ The median IFR was 0.0003% at 0–19 years, 0.002% at 20–29 years, 0.011% at 30–39 years, 0.035% at 40–49 years, 0.123% at 50–59 years, and 0.506% at 60–69 years.
∗ At a global level, pre-vaccination IFR may have been as low as 0.03% and 0.07% for 0–59 and 0–69 year old people, respectively.
∗ These IFR estimates in non-elderly populations are lower than previous calculations had suggested.
IFR
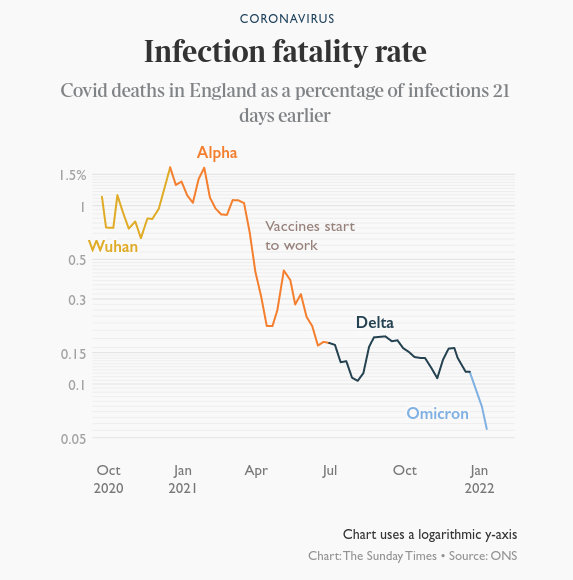
For most of the population, the infection fatality rate for COVID-19 is 0.03%-0.07%. Seasonal flu is around 0.1%-0.2%.

The vast majority of us have no risk of dying from COVID-19. Studies show that 99.94% survive COVID-19 and will be resistant for a long time. The QCovid risk calculator from Oxford University can be used to calculate your risk of death or hospitalisation.
Browse the articles related to this topic below.
Join our community on Guilded.
Across 31 systematically identified national seroprevalence studies in the pre-vaccination era, the median infection fatality rate of COVID-19 was estimated to be 0.035% for people aged 0-59 years people and 0.095% for those aged 0-69 years.
The median IFR was
* 0.0003% at 0-19 years
* 0.003% at 20-29 years
* 0.011% at 30-39 years
* 0.035% at 40-49 years
* 0.129% at 50-59 years
* and 0.501% at 60-69 years.At a global level, pre-vaccination IFR may have been as low as 0.03% and 0.07% for 0-59 and 0-69 year old people, respectively.
These IFR estimates in non-elderly populations are lower than previous calculations had suggested.
https://www.medrxiv.org/content/10.1101/2022.10.11.22280963v1
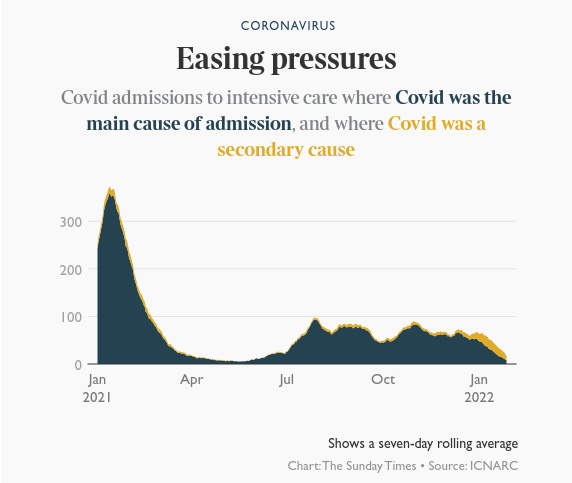
A report from the Intensive Care National Audit and Research Centre suggests a collapse in the number of patients becoming very unwell. It put the number of admissions to ICU of patients with Covid at 19 on January 23. About 400 people were being admitted daily at the peak of the second wave in January last year.
Here are key facts and sources about the alleged “pandemic”, that will help you get a grasp on what has happened to the world since January 2020, and help you enlighten any of your friends who might be still trapped in the New Normal fog.
- The survival rate of “Covid” is over 99%
- There has been NO unusual excess mortality
- “Covid death” counts are artificially inflated
- The vast majority of covid deaths have serious comorbidities
- Average age of “Covid death” is greater than the average life expectancy.
- Covid mortality exactly mirrors the natural mortality curve
- There has been a massive increase in the use of “unlawful” DNRs
- Lockdowns do not prevent the spread of disease
- Lockdowns kill people
- Hospitals were never unusually over-burdened
- PCR tests were not designed to diagnose illness
- PCR Tests have a history of being inaccurate and unreliable
- The CT values of the PCR tests are too high
- The World Health Organization (Twice) Admitted PCR tests produced false positives
- The scientific basis for Covid tests is questionable
- The majority of Covid infections are “asymptomatic”
- There is very little evidence supporting the alleged danger of “asymptomatic transmission”
- Ventilation is NOT a treatment for respiratory viruses
- Ventilators killed people
- Masks don’t work
- Masks are bad for your health
- Masks are bad for the planet
- Covid “vaccines” are totally unprecedented
- Vaccines do not confer immunity or prevent transmission
- The vaccines were rushed and have unknown longterm effects
- Vaccine manufacturers have been granted legal indemnity should they cause harm
- The EU was preparing “vaccine passports” at least a YEAR before the pandemic began
- A “training exercise” predicted the pandemic just weeks before it started
- Since the beginning of 2020, the Flu has “disappeared”
- The elite have made fortunes during the pandemic
/https://off-guardian.org/2021/09/22/30-facts-you-need-to-know-your-covid-cribsheet/
The elephants in the room – PANDA
While citizens focus on the latest issue the government directs our attention to, many of us have lost sight of the big picture and grown accustomed to severe limitations on our rights like the proverbial frogs in hot water. As a number of countries now seek to focus the discussion on further coercive measures and even mandatory vaccination, PANDA is increasingly aware of the elephants in the room, the topics no one is talking about.
http://archive.today/2021.09.16-104523/https://www.pandata.org/elephants-in-the-room/
“Lockdowns,” the mass quarantine of both sick and healthy people, have never before been used for disease mitigation in the modern Western world. Previously, the strategy had been systematically ruled out by the pandemic plans of the World Health Organization (WHO) and by health experts of every developed nation. So how did we get here?
https://www.tabletmag.com/sections/news/articles/masked-ball-cowardice
25 CYP died of SARS-CoV-2 during the first pandemic year in England, equivalent to an infection fatality rate of 5 per 100,000 and a mortality rate of 2 per million. Most had an underlying comorbidity, particularly neurodisability and life-limiting conditions. The CYP who died were mainly >10 years and of Asian and Black ethnicity, compared to other causes of the death, but their absolute risk of death was still extremely low.
Ivor Cummins aka the Fat Emperor – gives James the lowdown on why you can’t trust anything our governments tell us about Covid-19. If you want the facts on Coronavirus – how deadly is it? do lockdowns and masks work? how does it compare with previous pandemics? – you’ve come to the right place
Please support the Delingpod:
Mirror archives are available below if this video is removed from YouTube.
The SARS-CoV-2 Pandemic
In the interest of public debate, we allow visitors to share opinions, experiences and research that may be of value to others. This is a visitor contribution from our Discussions page.
The views expressed are those of the individual posters themselves. Please read our Comments and contributions disclaimer.
Author
George Michael
- Credentials: Physics graduate, University College London (UCL); Senior Research Analyst
- Contact: LinkedIn
The SARS-CoV-2 Pandemic
The COVID-19 pandemic has impacted the world at a horrific scale, and people are trying to form their own opinions — rightly so — on topics ranging from disease severity to government policy. However, the general public are not exposed to a consistent flow of reliable information, so many are suffering from fear, confusion, and isolation, exacerbated by extreme differences in opinion on how seriously any aspect of the pandemic should be taken. These are the problems that this report aims to address.
Read the full article on Medium: The SARS-CoV-2 Pandemic
Results
I included 61 studies (74 estimates) and eight preliminary national estimates. Seroprevalence estimates ranged from 0.02% to 53.40%. Infection fatality rates ranged from 0.00% to 1.63%, corrected values from 0.00% to 1.54%. Across 51 locations, the median COVID-19 infection fatality rate was 0.27% (corrected 0.23%): the rate was 0.09% in locations with COVID-19 population mortality rates less than the global average (< 118 deaths/million), 0.20% in locations with 118–500 COVID-19 deaths/million people and 0.57% in locations with > 500 COVID-19 deaths/million people. In people < 70 years, infection fatality rates ranged from 0.00% to 0.31% with crude and corrected medians of 0.05%.
Conclusion
The infection fatality rate of COVID-19 can vary substantially across different locations and this may reflect differences in population age structure and case-mix of infected and deceased patients and other factors. The inferred infection fatality rates tended to be much lower than estimates made earlier in the pandemic.
Accumulating data on deaths from covid-19 show an association with age that closely matches the “normal” risk we all face. Explaining risk in this way could help people understand and manage their response, says David Spiegelhalter
As covid-19 turns from a societal threat into a matter of risk management, it is vital that the associated risks are understood and clearly communicated.1 But these risks vary hugely between people, and so finding appropriate analogues is a challenge. Although covid-19 is a complex multisystem disease that can cause prolonged illness, here I focus solely on the risks of dying from covid-19 and explore the use of “normal” risk—the risk of death from all causes each year—as an aid to transparent communication.
- General population: the risk of catching and then dying from covid-19 during 16 weeks of the pandemic was equivalent to experiencing around 5 weeks extra “normal” risk for those over 55, decreasing steadily with age, to just 2 extra days for schoolchildren
- Over 55 who are infected with covid-19: additional risk of dying is slightly more than the “normal” risk of death from all other causes over one year, and less for under 55s.
But where did this one percent figure come from? You may find this hard to believe, but this figure emerged by mistake. A pretty major thing to make a mistake about, but that’s what happened.
In order to understand what happened, you have to understand the difference between two medical terms that sound the same – but are completely different. [IFR and CFR.]
CFR will always be far higher than the IFR. With influenza, the CFR is around ten times as high as the IFR. Covid seems to have a similar proportion.
Now, clearly, you do not want to get these figures mixed up. By doing so you would either wildly overestimate, or wildly underestimate, the impact of Covid. But mix these figures up, they did.
…we’ve had all the deaths we were ever going to get. And which also means that lockdown achieved, almost precisely nothing with regard to Covid. No deaths were prevented.
Our random-sample study estimated 187 802 cumulative infections, to which 180 hospitalizations were added. The average age among all COVID-19 decedents was 76.9 years (SD, 13.1). The overall noninstitutionalized IFR was 0.26%. In order of magnitude, the demographic-stratified IFR varied most by age, race, ethnicity, and sex. Persons younger than 40 years had an IFR of 0.01%; those aged 60 or older had an IFR of 1.71%. Whites had an IFR of 0.18%; non-Whites had an IFR of 0.59%.
By using SARS-CoV-2 population prevalence data, we found that the risk for death among infected persons increased with age. Indiana’s IFR for noninstitutionalized persons older than 60 years is just below 2% (1 in 50). In comparison, the ratio is approximately 2.5 times greater than the estimated IFR for seasonal influenza, 0.8% (1 in 125), among those aged 65 years and older. Of note, the IFR for non-Whites is more than 3 times that for Whites, despite COVID-19 decedents in that group being 5.6 years younger on average.
https://web.archive.org/web/20201003112851/https://www.acpjournals.org/doi/10.7326/M20-5352
2:55 – Masks
• Tom Jefferson: “Aside from people who are exposed on the frontlines, there is no evidence that masks make any difference, but what’s even more extraordinary is the uncertainty: we don’t know if these things make any difference…. We should have done randomised control trials in February, March and April but not anymore because viral circulation is low and we will need huge number of enrolees to show whether there was any difference”.
• Carl Heneghan: “By all means people can wear masks but they can’t say it’s an evidence-based decision… there is a real separation between an evidence-based decision and the opaque term that ‘we are being led by the science’, which isn’t the evidence”.
9:26 – Pandemic life cycle
• CH: “One of the keys of the infection is to look at who’s been infected, which shows a crucial difference when comparing the pandemic theory to seasonal theory. In a pandemic you’d expect to see young people disproportionately affected, but in the UK we’ve only had six child deaths, which is far less than we’d normally see in a pandemic. The high number of deaths with over-75s fits with the seasonal theory”.
14:00 – Covid seasonality
• CH: “The stability of the virus is far less when the temperature goes up but humidity seems to be particularly important. The lower the humidity, the more stable the virus is in the atmosphere and on surfaces… It’s now winter in the southern hemisphere, which is why places like Australia are suddenly having outbreaks.”
20:37 – Lockdown
• CH: “Many people said that we should have locked down earlier, but 50% of care homes developed outbreaks during the lockdown period so there are issues within the transmission of this virus that are not clear… Lockdown is a blunt tool and there needs to be intelligent conversations about what mitigation strategies can keep society functioning while we keep the most vulnerable shielded”.
25:20 – Nightingale hospitals
• CH: “They are the wrong structure. What you need is fever hospitals which were here until around the 1980s or 90s. They were on single floors and had isolation within isolation. Theere were no lift shafts and staff were trained, which meant that everyone was protected from each other… It looks like at leats 20% of people got the infection while they were in hospital”
27:30 – Suppression strategy
• CH: “The benefits of the current strategy are outweighed by the harms…When it comes to suppression, only the virus will have a determination in that. If you follow the New Zealand policy of suppressing it to zero and locking down the country forever, then you’re going to have a problem… This virus is so out there now, I cannot see a strategy that makes suppression the viable option. The strategy right now should be how we learn to live with this virus”
32:45 – Response to the virus
• TJ: “I am a survivor of four pandemics and for the other three, I didn’t even realise they were going on. People died but nothing changed and none of the fabric of society was eroded like this response… Do I see steps being taken at a European level about learning from our mistakes and changing policies? The answer is no…
39:30 – Politics of the virus
• CH: “We as individuals are part of the problem because sensationalism drives people to click and read the information. So it’s a big circle because we’ve created the problem — if we put the worst case scenario out there, we will go and have a look. If you want a solution, you’ve got to get people to stop clicking on this sensationalist stuff”.
43:30 – IFR
• CH: “We will be down about where we were with the swine flu: around 0.1-0.3% which is much lower than what we think because at the moment we are seeing the case fatality”.
• TJ: “If you look at the whole narrative, it was distorted from the very beginning by the obsession with influenza which was just one or two agents and nothing else existed. We’re no different now”.