- Misinformation #1: Natural immunity offers little protection compared to vaccinated immunity
- Misinformation #2: Masks prevent Covid transmission
- Misinformation #3: School closures reduce Covid transmission
- Misinformation #5: Young people benefit from a vaccine booster
- Misinformation #6: Vaccine mandates increased vaccination rates
- Misinformation #7: Covid originating from the Wuhan Lab is a conspiracy theory
- Misinformation #8: It was important to get the 2nd vaccine dose 3 or 4 weeks after the 1st dose
- Misinformation #8: It was important to get the 2nd vaccine dose 3 or 4 weeks after the 1st dose
- Misinformation #9: Data on the bivalent vaccine is “crystal clear”
- Misinformation #10: One in five people get long Covid
Public Health
Browse the articles related to this topic below.
Join our community on Guilded.
I was wrong. We in the scientific community were wrong. And it cost lives.
I can see now that the scientific community from the CDC to the WHO to the FDA and their representatives, repeatedly overstated the evidence and misled the public about its own views and policies, including on natural vs. artificial immunity, school closures and disease transmission, aerosol spread, mask mandates, and vaccine effectiveness and safety, especially among the young. All of these were scientific mistakes at the time, not in hindsight. Amazingly, some of these obfuscations continue to the present day.
Up to 100 times more may have been spent on preventing each Covid death than on preventing each non-Covid death
- UK shows an alarming increase in non-Covid related excess deaths.
- This is consistent with data from November 2022.
- This merits an official government response.
- Data shows there are more infections but fewer cases are symptomatic, which is good news.
- Infections are high but hospitalisations are not high.
- Deaths due to Covid are not increasing. It’s the non-Covid deaths that are increasing.
- Previous infections reduce the likelihood of getting re-infected.
- Protection from the vaccine against re-infection only lasts 10-11 weeks, which is not very long.
- Most people admitted to hospital as incidental infections (not admitted for Covid).
- We’re not seeing many deaths in younger age groups.
- Other than age, obesity is the biggest risk factor of dying from Covid.
- It is strange that the government is not talking about these excess deaths which would constitute a public health emergency.
To help society mount a collective defence against pathogens, researchers say that leaders should enlist human-behaviour specialists to play a much bigger part in health policy. This has been the Achilles heel of governments during the COVID-19 pandemic, says Armand Balboni, an infectious-disease researcher and chief executive of pharmaceutical firm Appili Therapeutics in Halifax, Canada. “Social scientists, anthropologists and psychologists were not used nearly enough,” Balboni says.
http://archive.today/2022.11.15-082310/https://www.nature.com/articles/d41586-022-03354-8
…It also brings the recommendations for unvaccinated people in line with people who are fully vaccinated – an acknowledgment of the high levels of population immunity in the U.S., due to vaccination, past COVID-19 infections or both. “Based on the latest … data, it’s around 95% of the population,” Massetti said, “And so it really makes the most sense to not differentiate,” since many people have some protection against severe disease.
To prevent medically significant COVID-19 illness and death, persons must understand their risk, take steps to protect themselves and others with vaccines, therapeutics, and nonpharmaceutical interventions when needed, receive testing and wear masks when exposed, receive testing if symptomatic, and isolate for ≥5 days if infected.
http://archive.today/2022.08.12-074019/https://www.cdc.gov/mmwr/volumes/71/wr/mm7133e1.htm
Abstract
The present coronavirus crisis caused a major worldwide disruption which has not been experienced for decades. The lockdown-based crisis management was implemented by nearly all the countries, and studies confirming lockdown effectiveness can be found alongside the studies questioning it. In this work, we performed a narrative review of the works studying the above effectiveness, as well as the historic experience of previous pandemics and risk-benefit analysis based on the connection of health and wealth. Our aim was to learn lessons and analyze ways to improve the management of similar events in the future. The comparative analysis of different countries showed that the assumption of lockdowns’ effectiveness cannot be supported by evidence—neither regarding the present COVID-19 pandemic, nor regarding the 1918–1920 Spanish Flu and other less-severe pandemics in the past. The price tag of lockdowns in terms of public health is high: by using the known connection between health and wealth, we estimate that lockdowns may claim 20 times more life years than they save. It is suggested therefore that a thorough cost-benefit analysis should be performed before imposing any lockdown for either COVID-19 or any future pandemic.
Conclusions
While our understanding of viral transmission mechanisms leads to the assumption that lockdowns may be an effective pandemic management tool, this assumption cannot be supported by the evidence-based analysis of the present COVID-19 pandemic, as well as of the 1918–1920 H1N1 influenza type-A pandemic (the Spanish Flu) and numerous less-severe pandemics in the past. The price tag of lockdowns in terms of public health is high: we estimate that, even if somewhat effective in preventing death caused by infection, lockdowns may claim 20 times more life than they save. It is suggested therefore that a thorough cost-benefit analysis should be performed before imposing any lockdown in the future.
Published September 2018
The behavioural and social sciences are the future of public health. Evidence from behavioural science suggests that simple and easy ways of helping people to change their behaviour are the most effective. Whether it’s encouraging smokers to quit, increasing uptake of the NHS Health Check, making healthier food choices easier, or reducing the number of inappropriate antibiotic prescriptions, this evidence can help in understanding and therefore influencing behaviour change that promotes health, prevents disease, and reduces health inequalities. We must reach and be meaningful to people in the lives that they are leading.
It is time for the public health system to advance the use of behavioural and social sciences, and for this purpose, PHE’s Behavioural Insights experts, working with many partners, have led the collaborative development of this comprehensive strategy – the first of its kind in the field.
For commentary on this document, see UK Column News, 23rd February 2022.
The World Health Organization amplified false Chinese statements about COVID-19 initially, while it dragging its feet on declaring an international emergency. Pandemic experts here clung to flu epidemic plans too, ignoring observable COVID-19 successes in East Asia and so ruling out any similar possibility of test-and-trace containment in the UK from the off.
Most public health experts then pivoted to being extremely pro-lockdown, but stuck rigidly to this even as the context, and so the costs and benefits of restrictions, changed with the vaccines and omicron.
Epidemiologists proved especially stubborn. Their modelling usually ignored the role of voluntary behavioural change entirely, so erred on the side of assuming catastrophic public health outcomes absent government mandates and restrictions. Hence, Freedom Day was dubbed “criminal” by scientists, while the government’s scientific advisers called for more restrictions last Christmas. Both proved wrong in retrospect.
It seems obvious that wherever vaccine mandates, mask mandates, and lockdowns have been imposed in response to covid-19, progressive political and media elites have been the driving forces behind them. This is clear to those of us alive today, but it is worth considering whether future history books will attempt to erase progressives’ culpability for the disasters their covid policies have caused. The argument that follows is speculative, but bad ideologies should be held to the fires of their own making, and it seems to be in the nature of progressivism to attempt to escape the historical reckoning it is due.
https://mises.org/wire/how-progressives-will-write-history-covid
Were masks a waste of time? – UnHerd
Two years into the pandemic, the experts are now the last to acknowledge the accuracy of their earlier predictions. This raises the question of why they changed course and sacrificed their own credibility in the process. Miller confines himself to the data, and if there’s a limitation to his book, it’s that he does not offer any compelling explanation of why the expert class threw itself a policy it once regarded as worse than useless.
It is not difficult to see why mask mandates proved irresistible to politicians. Masks are the perfect form of hygiene theatre, conveying an intuitive sense of safety regardless of demonstrable efficacy at scale. They also offload responsibility for controlling the pandemic to ordinary people. The overcrowding of ICUs can be blamed on the bad behavior of “anti-maskers”, rather than on the allocation of resources by governments and hospital CEOs. When cases and deaths spike, it is the fault of the citizenry, not the leadership.
The scientific and medical establishment’s uncritical support of masks and other dubious policies is just the latest manifestation of its lack of independence from political imperatives. After several years of finding themselves at the receiving end of rhetorical assaults from rising Right-wing populists, the experts seized on the pandemic as an opportunity to reassert their own status and authority — and that of the liberal-technocratic politicians with whom they are largely aligned.
http://archive.today/2022.02.07-062226/https://unherd.com/2022/02/were-masks-a-waste-of-time/
One of the checks and balances on rampant bad scientific research is to continuously assess how new ideas fit into the framework of the bigger picture. A new piece of information may seem perfectly reasonable and well-documented, but the domino effect of its implications gives you another way to test its validity. When multiple lines of seemingly rock-solid evidence contradict one another, that’s a good sign that something is wrong, even if you don’t yet know why. Whenever a thread seems out of place, it’s time to pull on that thread until you can figure out what exactly is going on.
…”Trusting the science” is not (and never has been) about trusting results or trusting experts. Trusting the scientists is what got us into this mess. For science to function properly, we must NOT trust the scientists. Instead, we must trust in the messy self-correcting process that allows truth to boil to the surface even if every participant in that process is flawed.
“Science is the belief in the ignorance of the Experts”
— Richard P. FeynmanScience is the relentless competition between measurable pieces of evidence, the ruthless gauntlet of debate, the willingness to question even the most “obvious” of assumptions, and the humbleness to test and retest any and all assumptions against hard evidence, most especially when those assumptions are our own.
https://www.juliusruechel.com/2022/01/who-do-you-trust-if-you-cant-trust.html
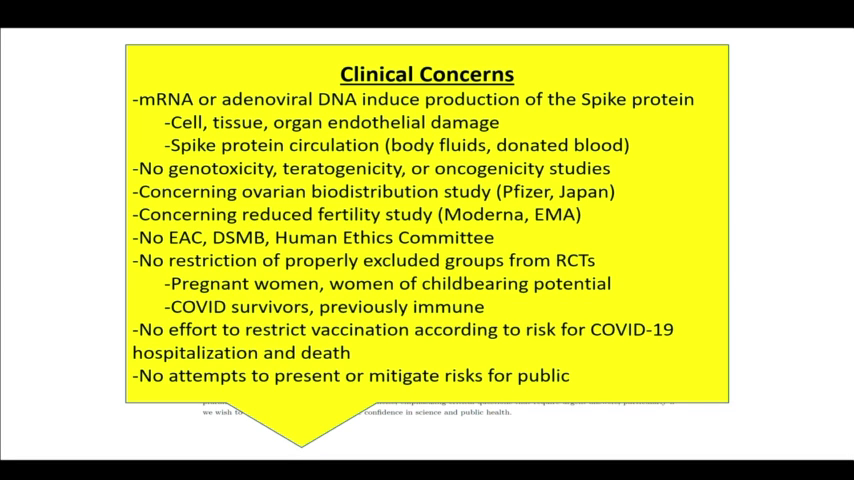
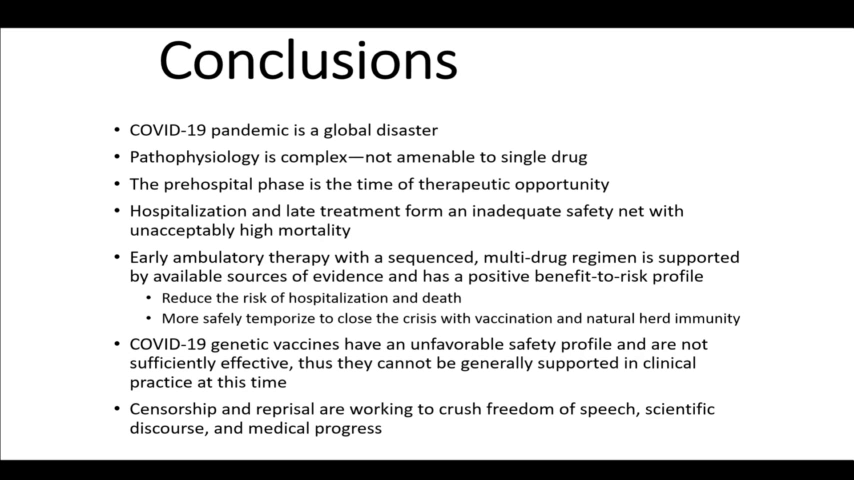
Peter McCullough, MD, MPH speaks at the 78th Annual Meeting of AAPS on October 2, 2021.
Presentation notes:
- 1min: Something was going very wrong very early in 2019.
- 2m: The threshold for shutting down a new biologic product is just a few cases.
- 3m: Covid-19 was going to be the showcase of what we could do for biotech.
- 5m: The spike protein created by the new Covid-19 is a deadly protein.
- 11m: Our institutions are all culpable in medical malfeasance.
- 13m: We have the biggest biological catastrophe on our hands with a medicinal product in human history…and no-one knows how to stop it.
- List of risk
- 14m: 86% of deaths have no other explanation other than the vaccines.
- 20m: We are in freefall into a lawless state. The Vaccines are not safe for use on either side of the Atlantic. It’s clear that this first generation of [Covid-19] vaccines is not safe.
- 22m: The FDA did not approve Pfizer. The gave a continuation of the emergency use authorization and then conditionally approved Comirnaty with BioNTech which is legally and potentially medicinally distinct. The Pfizer approval is a false talking point.
- 23m: When Pfizer came up for boosters, McCullough and his team presented at the FDA showing that death with the vaccine is greater than death just taking your chances with the infection. The vaccines aren’t safe across the board and the panel agreed 16:2 against the booster.
- 26m: Data for the efficacy of the vaccines do not take into account the Delta variant. These vaccines have failed against Delta and other variants. Two-thirds who get sick with Delta are fully vaccinated. Data shows that the vaccines can’t stop transmission.
- 27m: Effectiveness for Pfizer is at 42%. A vaccine that falls below 50% protection and can’t last a year is not a viable product. Pfizer has failed as a commercial product.
- 29m: The CDC was telling us in May 2021 that the vaccines were failing. They started to do asymmetric reporting to craft a narrative that this was going to be a crisis of the unvaccinated but the CDC data showed the opposite. The ineptitude and willful misconduct of the people running our public health agencies is astounding.
- 32m: The ‘99% of hospitalized were unvaccinated’ message was a propagandized false talking point because the data is not there.
- 33m: The vaccines have had zero impact on the epidemic curve. Mortality is a function of treatment.
- 34m: Many experts have been warning that we shouldn’t vaccinate into a pandemic because it creates resistance. As soon as we started vaccinating, the number of strains starting falling. The virus was figuring out how to thrive in the vaccinated.
- 36m: The Delta variant has achieved antigenic escape. The data shows that the vaccinated is an equal threat to the unvaccinated.
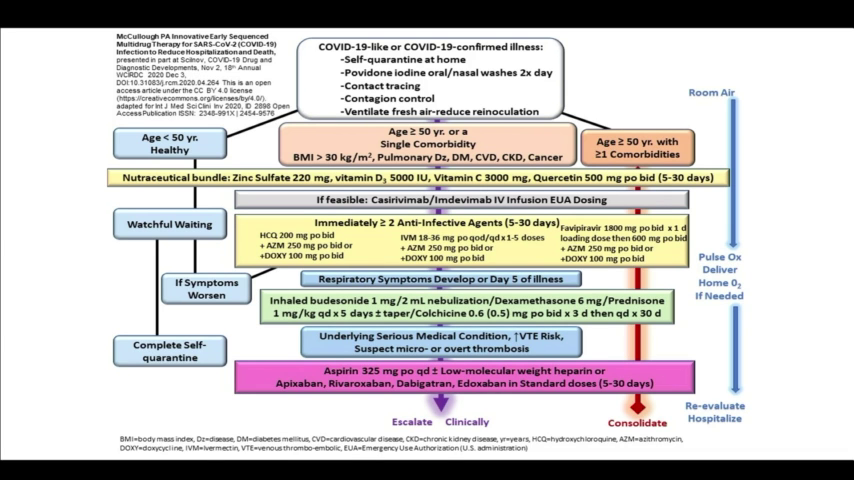
- 38m: Early home treatment is the only thing that makes sense. That’s what it should have always been.
- 40m: Doctors at my institution cannot look me in the eye because they are so ashamed of what they’ve done during the course of this pandemic.
- 44m: If you look through the clinical records [of those who have died] and I will tell you they were all inadequately treated.
- 50m: Natural immunity is superior to vaccine immunity. If we vaccinate people who are covid-recovered, we harm them considerably. The only backstop is natural immunity.
File download:
A Guide to Home-Based COVID Treatment from the Association of American Physicians and Surgeons – PDF (1.4MiB)
Slides:
Backup mirrors:
Government agencies such as health departments might be more inclined to intervene if findings from a study they commissioned are not as expected or if they are heavily invested in the health intervention — such as an education or health programme — being trialled, she adds.
A 2016 inquiry into the delayed publication of research commissioned by UK government agencies identified cases in which publication was “manipulated to fit with political concerns”. More recently, the British Medical Journal reported four instances of politicization and suppression of science in the United Kingdom during the COVID-19 pandemic.

http://archive.today/2021.08.20-134039/https://www.nature.com/articles/d41586-021-02242-x
I had no choice but to speak out against lockdowns. As a public-health scientist with decades of experience working on infectious-disease outbreaks, I couldn’t stay silent. Not when basic principles of public health are thrown out of the window. Not when the working class is thrown under the bus. Not when lockdown opponents were thrown to the wolves. There was never a scientific consensus for lockdowns. That balloon had to be popped.
…Ultimately, lockdowns protected young low-risk professionals working from home – journalists, lawyers, scientists, and bankers – on the backs of children, the working class and the poor.
https://www.spiked-online.com/2021/06/04/why-i-spoke-out-against-lockdowns/
Dr. Jay Bhattacharya, a professor at Stanford University Medical School, recently said that COVID-19 lockdowns are the “biggest public health mistake we’ve ever made…The harm to people is catastrophic.”
“I stand behind my comment that the lockdowns are the single worst public health mistake in the last 100 years. We will be counting the catastrophic health and psychological harms, imposed on nearly every poor person on the face of the earth, for a generation.
At the same time, they have not served to control the epidemic in the places where they have been most vigorously imposed. In the US, they have – at best – protected the ‘non-essential’ class from COVID, while exposing the essential working class to the disease. The lockdowns are trickle down epidemiology.“
In this article, we aim to develop a political economy of mass hysteria. Using the background of COVID-19, we study past mass hysteria. Negative information which is spread through mass media repetitively can affect public health negatively in the form of nocebo effects and mass hysteria. We argue that mass and digital media in connection with the state may have had adverse consequences during the COVID-19 crisis. The resulting collective hysteria may have contributed to policy errors by governments not in line with health recommendations. While mass hysteria can occur in societies with a minimal state, we show that there exist certain self-corrective mechanisms and limits to the harm inflicted, such as sacrosanct private property rights. However, mass hysteria can be exacerbated and self-reinforcing when the negative information comes from an authoritative source, when the media are politicized, and social networks make the negative information omnipresent. We conclude that the negative long-term effects of mass hysteria are exacerbated by the size of the state.
http://archive.today/2021.02.09-004023/https://www.mdpi.com/1660-4601/18/4/1376/htm
You may realise my personification of the NHS, referring to it as she and her. Why? Well, the narrative of the NHS is the narrative of all of us. How many of us were born in an NHS hospital? How many of our lives and our family’s lives has she saved? The NHS is more than a set of buildings or a mere organisation; she is every one of us. A living, breathing establishment made up of 1.5 million dedicated workers, 66.6m patients. She is ours, and we are hers.
Increasing COVID-19 caseloads were associated with countries with higher obesity (adjusted rate ratio [RR]=1.06; 95%CI: 1.01–1.11), median population age (RR=1.10; 95%CI: 1.05–1.15) and longer time to border closures from the first reported case (RR=1.04; 95%CI: 1.01–1.08). Increased mortality per million was significantly associated with higher obesity prevalence (RR=1.12; 95%CI: 1.06–1.19) and per capita gross domestic product (GDP) (RR=1.03; 95%CI: 1.00–1.06). Reduced income dispersion reduced mortality (RR=0.88; 95%CI: 0.83–0.93) and the number of critical cases (RR=0.92; 95% CI: 0.87–0.97). Rapid border closures, full lockdowns, and wide-spread testing were not associated with COVID-19 mortality per million people. However, full lockdowns (RR=2.47: 95%CI: 1.08–5.64) and reduced country vulnerability to biological threats (i.e. high scores on the global health security scale for risk environment) (RR=1.55; 95%CI: 1.13–2.12) were significantly associated with increased patient recovery rates.
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30208-X/fulltext