From January 21 through February 23, 2020, public health agencies detected 14 U.S. cases of coronavirus disease 2019 (COVID-19), all related to travel from China (1,2). The first nontravel–related U.S. case was confirmed on February 26 in a California resident who had become ill on February 13 (3). Two days later, on February 28, a second nontravel–related case was confirmed in the state of Washington (4,5). Examination of four lines of evidence provides insight into the timing of introduction and early transmission of SARS-CoV-2, the virus that causes COVID-19, into the United States before the detection of these two cases. First, syndromic surveillance based on emergency department records from counties affected early by the pandemic did not show an increase in visits for COVID-19–like illness before February 28. Second, retrospective SARS-CoV-2 testing of approximately 11,000 respiratory specimens from several U.S. locations beginning January 1 identified no positive results before February 20. Third, analysis of viral RNA sequences from early cases suggested that a single lineage of virus imported directly or indirectly from China began circulating in the United States between January 18 and February 9, followed by several SARS-CoV-2 importations from Europe. Finally, the occurrence of three cases, one in a California resident who died on February 6, a second in another resident of the same county who died February 17, and a third in an unidentified passenger or crew member aboard a Pacific cruise ship that left San Francisco on February 11, confirms cryptic circulation of the virus by early February. These data indicate that sustained, community transmission had begun before detection of the first two nontravel–related U.S. cases, likely resulting from the importation of a single lineage of virus from China in late January or early February, followed by several importations from Europe. The widespread emergence of COVID-19 throughout the United States after February highlights the importance of robust public health systems to respond rapidly to emerging infectious threats.
Publications
An archive of industry publications, scientific journals and officially-released data.
Browse the articles related to this topic below.
Join our community on Guilded.
“90 percent or more of SARS-CoV-2 virus will be inactivated after being exposed [to summer sun] for 11 to 34 minutes.”
Using a model developed for estimating solar inactivation of viruses of biodefense concerns, we calculated the expected inactivation of SARS-CoV-2 virus, cause of COVID-19 pandemic, by artificial UVC and by solar ultraviolet radiation in several cities of the world during different times of the year. The UV sensitivity estimated here for SARS-CoV-2 is compared with those reported for other ssRNA viruses, including influenza A virus. The results indicate that SARS-CoV-2 aerosolized from infected patients and deposited on surfaces could remain infectious outdoors for considerable time during the winter in many temperate-zone cities, with continued risk for re-aerosolization and human infection. Conversely, the presented data indicate that SARS-CoV-2 should be inactivated relatively fast (faster than influenza A) during summer in many populous cities of the world, indicating that sunlight should have a role in the occurrence, spread rate, and duration of coronavirus pandemics.
COVID-19 appears to follow the Gompertz curve in every outbreak region. This means that government interventions do nothing to stop the virus.
We demonstrate that universal scaling behavior is observed in the current coronavirus (COVID-19) spread in various countries. We analyze the numbers of infected people in selected eleven countries (Japan, USA, Russia, Brazil, China, Italy, Indonesia, Spain,South Korea, UK, and Sweden). By using the double exponential function called the Gompertz function, fG(x)=exp(−e−x), the number of infected people is well described as N(t)=N0 fG(γ(t−t0)), where N0, γ and t0 are the final total number of infected people, the damping rate of the infection probability and the peak time of dN(t)/dt, respectively. The scaled data of infected people in most of the analyzed countries are found to collapse onto a common scaling function fG(x) with x=γ(t−t0) in the range of fG(x) ± 0.05. The recently proposed indicator so-called the K value, the increasing rate of infected people in one week, is also found to show universal behavior. The mechanism for the Gompertz function to appear is discussed from the time dependence of the produced pion numbers in nucleus-nucleus collisions, which is also found to be described by the Gompertz function.
https://www.medrxiv.org/content/10.1101/2020.06.18.20135210v1
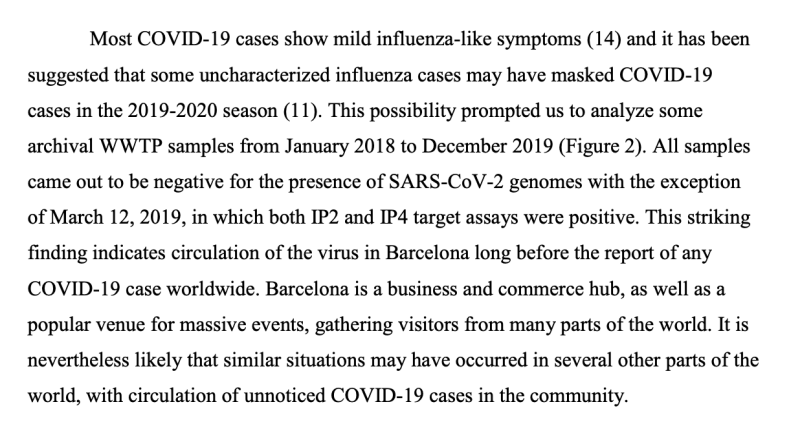
SARS-CoV-2 was detected in Barcelona sewage long before the declaration of the first COVID-19 case, indicating that the infection was present in the population before the first imported case was reported. Sentinel surveillance of SARS-CoV-2 in wastewater would enable adoption of immediate measures in the event of future COVID-19 waves.
https://www.medrxiv.org/content/10.1101/2020.06.13.20129627v1
A Mystery of the Gompertz Function
The Gompertz function describes global dynamics of many natural processes including growth of normal and malignant tissues. On one hand, the Gompertz function defines a fractal. The fractal structure of time-space is a prerequisite condition for the coupling and Gompertzian growth. On the other hand, the Gompertz function is a probability function. Its derivative is a probability density function. Gompertzian dynamics emerges as a result of the co-existence of at least two antagonistic processes with the complex coupling of their probabilities. This dynamics implicates a coupling between time and space through a linear function of their logarithms. The spatial fractal dimension is a function of both scalar time and the temporal fractal dimension. The Gompertz function reflects the equilibrium between regular states with predictable dynamics and chaotic states with unpredictable dynamics; a fact important for cancer chemoprevention. We conclude that the fractal-stochastic dualism is a universal natural law of biological complexity.
Working safely during COVID-19 in offices and contact centres, published 24 June 2020, states:
6. Personal Protective Equipment (PPE) and face coverings
(Emphasis mine)
Unless you are in a situation where the risk of COVID-19 transmission is very high, your risk assessment should reflect the fact that the role of PPE in providing additional protection is extremely limited.
6.1 Face coverings
There are some circumstances when wearing a face covering may
be marginally beneficial as a precautionary measure. The evidence
suggests that wearing a face covering does not protect you, but it
may protect others if you are infected but have not developed
symptoms.
It is important to know that the evidence of the benefit of using a face covering to protect others is weak and the effect is likely to be small…

Advice for offices and contact centres: https://assets.publishing.service.gov.uk/media/5eb97e7686650c278d4496ea/working-safely-during-covid-19-offices-contact-centres-240620.pdf
Advice for restaurants, pubs, bars and takeaway services: https://assets.publishing.service.gov.uk/media/5eb96e8e86650c278b077616/Keeping-workers-and-customers-safe-during-covid-19-restaurants-pubs-bars-takeaways-230620.pdf
Advice for close contact services: https://assets.publishing.service.gov.uk/media/5ef2889986650c12970e9b57/Keeping-workers-and-clients-safe-during-covid-19-close-contact-services-230620.pdf
There were 3 influenza pandemics in the 20th century, and there has been 1 so far in the 21st century. Local, national, and international health authorities regularly update their plans for mitigating the next influenza pandemic in light of the latest available evidence on the effectiveness of various control measures in reducing transmission. Here, we review the evidence base on the effectiveness of nonpharmaceutical personal protective measures and environmental hygiene measures in nonhealthcare settings and discuss their potential inclusion in pandemic plans. Although mechanistic studies support the potential effect of hand hygiene or face masks, evidence from 14 randomized controlled trials of these measures did not support a substantial effect on transmission of laboratory-confirmed influenza. We similarly found limited evidence on the effectiveness of improved hygiene and environmental cleaning. We identified several major knowledge gaps requiring further research, most fundamentally an improved characterization of the modes of person-to-person transmission.
Note: This article, published on 16 October 2016, originally appeared in the Oral Health website. It was removed sometime after the end of June 2020 with no explanation other than, it being ‘no longer relevant in our current climate.’
The science behind face masks has not changed considerably in the past few months so we can only guess about what ‘no longer relevant’ means.
While you can find a capture at archive.org, we have saved a copy here to protect against censorship and for easy sharing.
Yesterday’s Scientific Dogma is Today’s Discarded Fable
Introduction
The above quotation is ascribed to Justice Archie Campbell author of Canada’s SARS Commission Final Report. 1 It is a stark reminder that scientific knowledge is constantly changing as new discoveries contradict established beliefs. For at least three decades a face mask has been deemed an essential component of the personal protective equipment worn by dental personnel. A current article, “Face Mask Performance: Are You Protected” gives the impression that masks are capable of providing an acceptable level of protection from airborne pathogens. 2 Studies of recent diseases such as Severe Acute Respiratory Syndrome (SARS), Middle Eastern Respiratory Syndrome (MERS) and the Ebola Crisis combined with those of seasonal influenza and drug resistant tuberculosis have promoted a better understanding of how respiratory diseases are transmitted. Concurrently, with this appreciation, there have been a number of clinical investigations into the efficacy of protective devices such as face masks. This article will describe how the findings of such studies lead to a rethinking of the benefits of wearing a mask during the practice of dentistry. It will begin by describing new concepts relating to infection control especially personal protective equipment (PPE).
Trends in Infection Control
For the past three decades there has been minimal opposition to what have become seemingly established and accepted infection control recommendations. In 2009, infection control specialist Dr. D. Diekema questioned the validity of these by asking what actual, front-line hospital-based infection control experiences were available to such authoritative organization as the Centers for Disease Control and Prevention (CDC), the Occupational Safety and Health Association (OSHA) and the National Institute for Occupational Safety and Health (NIOSH). 3 In the same year, while commenting on guidelines for face masks, Dr. M. Rupp of the Society for Healthcare Epidemiology of America noted that some of the practices relating to infection control that have been in place for decades, ”haven’t been subjected to the same strenuous investigation that, for instance, a new medicine might be subjected.” 4 He opined that perhaps it is the relative cheapness and apparent safety of face masks that has prevented them from undergoing the extensive studies that should be required for any quality improvement device. 4 More recently, Dr. R. MacIntyre, a prolific investigator of face masks, has forcefully stated that the historical reliance on theoretical assumptions for recommending PPEs should be replaced by rigorously acquired clinical data. 5 She noted that most studies on face masks have been based on laboratory simulated tests which quite simply have limited clinical applicability as they cannot account for such human factors as compliance, coughing and talking. 5
Covering the nose and mouth for infection control started in the early 1900s when the German physician Carl Flugge discovered that exhaled droplets could transmit tuberculosis. 4 The science regarding the aerosol transmission of infectious diseases has, for years, been based on what is now appreciated to be “very outmoded research and an overly simplistic interpretation of the data.” 6 Modern studies are employing sensitive instruments and interpretative techniques to better understand the size and distribution of potentially infectious aerosol particles. 6 Such knowledge is paramount to appreciating the limitations of face masks. Nevertheless, it is the historical understanding of droplet and airborne transmission that has driven the longstanding and continuing tradition of mask wearing among health professionals. In 2014, the nursing profession was implored to “stop using practice interventions that are based on tradition” but instead adopt protocols that are based on critical evaluations of the available evidence. 7
A December 2015 article in the National Post seems to ascribe to Dr. Gardam, Director of Infection Prevention and Control, Toronto University Health Network the quote, “I need to choose which stupid, arbitrary infection control rules I’m going to push.” 8 In a communication with the author, Dr. Gardam explained that this was not a personal belief but that it did reflect the views of some infection control practitioners. In her 2014 article, “Germs and the Pseudoscience of Quality Improvement”, Dr. K Sibert, an anaesthetist with an interest in infection control, is of the opinion that many infection control rules are indeed arbitrary, not justified by the available evidence or subjected to controlled follow-up studies, but are devised, often under pressure, to give the appearance of doing something. 9
The above illustrate the developing concerns that many infection control measures have been adopted with minimal supporting evidence. To address this fault, the authors of a 2007 New England Journal of Medicine (NEJM) article eloquently argue that all safety and quality improvement recommendations must be subjected to the same rigorous testing as would any new clinical intervention. 10 Dr. R. MacIntyre, a proponent of this trend in infection control, has used her research findings to boldly state that, “it would not seem justifiable to ask healthcare workers to wear surgical masks.” 4 To understand this conclusion it is necessary to appreciate the current concepts relating to airborne transmissions.
Airborne Transmissions
Early studies of airborne transmissions were hampered by the fact that the investigators were not able to detect small particles (less than 5 microns) near an infectious person. 6 Thus, they assumed that it was the exposure of the face, eyes and nose to large particles (greater than 5 microns) or “droplets” that transmitted the respiratory condition to a person in close proximity to the host. 6 This became known as “droplet infection”, and 5 microns or greater became established as the size of large particles and the traditional belief that such particles could, in theory, be trapped by a face mask. 5 The early researchers concluded that since only large particles were detected near an infectious person any small particles would be transmitted via air currents, dispersed over long distances, remain infective over time and might be inhaled by persons who never had any close contact with the host. 11 This became known as “airborne transmission” against which a face mask would be of little use. 5
Through the use of highly sensitive instruments it is now appreciated that the aerosols transmitted from the respiratory tract due to coughing, sneezing, talking, exhalation and certain medical and dental procedures produce respiratory particles that range from the very small (less than 5 microns) to the very large (greater than a 100 microns) and that all of these particles are capable of being inhaled by persons close to the source. 6, 11 This means that respiratory aerosols potentially contain bacteria averaging in size from 1-10 microns and viruses ranging in size from 0.004 to 0.1 microns. 12 It is also acknowledged that upon their emission large “droplets” will undergo evaporation producing a concentration of readily inhalable small particles surrounding the aerosol source. 6
The historical terms “droplet infection” and “airborne transmission” defined the routes of infection based on particle size. Current knowledge suggests that these are redundant descriptions since aerosols contain a wide distribution of particle sizes and that they ought to be replaced by the term, “aerosol transmissible.” 4, 5 Aerosol transmission has been defined as “person –to – person transmission of pathogens through air by means of inhalation of infectious particles.” 26 In addition, it is appreciated that the physics associated with the production of the aerosols imparts energy to microbial suspensions facilitating their inhalation. 11
Traditionally face masks have been recommended to protect the mouth and nose from the “droplet” route of infection, presumably because they will prevent the inhalation of relatively large particles. 11 Their efficacy must be re-examined in light of the fact that aerosols contain particles many times smaller than 5 microns. Prior to this examination, it is pertinent to review the defence mechanism of the respiratory tract.
Respiratory System Defences
Comprehensive details on the defence mechanisms of the respiratory tract will not be discussed. Instead readers are reminded that; coughing, sneezing, nasal hairs, respiratory tract cilia, mucous producing lining cells and the phagocytic activity of alveolar macrophages provide protection against inhaled foreign bodies including fungi, bacteria and viruses. 13 Indeed, the pathogen laden aerosols produced by everyday talking and eating would have the potential to cause significant disease if it were not for these effective respiratory tract defences.
These defences contradict the recently published belief that dentally produced aerosols, “enter unprotected bronchioles and alveoli.” 2 A pertinent demonstration of the respiratory tract’s ability to resist disease is the finding that- compared to controls- dentists had significantly elevated levels of antibodies to influenza A and B and the respiratory syncytial virus. 14 Thus, while dentists had greater than normal exposure to these aerosol transmissible pathogens, their potential to cause disease was resisted by respiratory immunologic responses. Interestingly, the wearing of masks and eye glasses did not lessen the production of antibodies, thus reducing their significance as personal protective barriers. 14 Another example of the effectiveness of respiratory defences is that although exposed to more aerosol transmissible pathogens than the general population, Tokyo dentists have a significantly lower risk of dying from pneumonia and bronchitis. 15 The ability of a face mask to prevent the infectious risk potentially inherent in sprays of blood and saliva reaching the wearers mouth and nose is questionable since, before the advent of mask use, dentists were no more likely to die of infectious diseases than the general population. 16
The respiratory tract has efficient defence mechanisms. Unless face masks have the ability to either enhance or lessen the need for such natural defences, their use as protection against airborne pathogens must be questioned.
Face Masks
History: Cloth or cotton gauze masks have been used since the late 19th century to protect sterile fields from spit and mucous generated by the wearer. 5,17,18 A secondary function was to protect the mouth and nose of the wearer from the sprays and splashes of blood and body fluids created during surgery. 17 As noted above, in the early 20th century masks were used to trap infectious “droplets” expelled by the wearer thus possibly reducing disease transmission to others. 18 Since the mid-20th century until to-day, face masks have been increasingly used for entirely the opposite function: that is to prevent the wearer from inhaling respiratory pathogens. 5,20,21 Indeed, most current dental infection control recommendations insist that a face mask be worn, “as a key component of personal protection against airborne pathogens”. 2
Literature reviews have confirmed that wearing a mask during surgery has no impact whatsoever on wound infection rates during clean surgery. 22,23,24,25,26 A recent 2014 report states categorically that no clinical trials have ever shown that wearing a mask prevents contamination of surgical sites. 26 With their original purpose being highly questionable it should be no surprise that the ability of face masks to act as respiratory protective devices is now the subject of intense scrutiny. 27 Appreciating the reasons for this, requires an understanding of the structure, fit and filtering capacity of face masks.
Structure and Fit: Disposable face masks usually consist of three to four layers of flat non-woven mats of fine fibres separated by one or two polypropylene barrier layers which act as filters capable of trapping material greater than 1 micron in diameter. 18,24,28 Masks are placed over the nose and mouth and secured by straps usually placed behind the head and neck. 21 No matter how well a mask conforms to the shape of a person’s face, it is not designed to create an air tight seal around the face. Masks will always fit fairly loosely with considerable gaps along the cheeks, around the bridge of the nose and along the bottom edge of the mask below the chin. 21 These gaps do not provide adequate protection as they permit the passage of air and aerosols when the wearer inhales. 11,17 It is important to appreciate that if masks contained filters capable of trapping viruses, the peripheral gaps around the masks would continue to permit the inhalation of unfiltered air and aerosols. 11
Filtering Capacity: The filters in masks do not act as sieves by trapping particles greater than a specific size while allowing smaller particles to pass through. 18 Instead the dynamics of aerosolized particles and their molecular attraction to filter fibres are such that at a certain range of sizes both large and small particles will penetrate through a face mask. 18 Accordingly, it should be no surprise that a study of eight brands of face masks found that they did not filter out 20-100% of particles varying in size from 0.1 to 4.0 microns. 21 Another investigation showed penetration ranges from 5-100% when masks were challenged with relatively large 1.0 micron particles. 29 A further study found that masks were incapable of filtering out 80-85% of particles varying in size from 0.3 to 2.0 microns. 30 A 2008 investigation identified the poor filtering performance of dental masks. 27 It should be concluded from these and similar studies that the filter material of face masks does not retain or filter out viruses or other submicron particles. 11,31 When this understanding is combined with the poor fit of masks, it is readily appreciated that neither the filter performance nor the facial fit characteristics of face masks qualify them as being devices which protect against respiratory infections. 27 Despite this determination the performance of masks against certain criteria has been used to justify their effectiveness.2 Accordingly, it is appropriate to review the limitations of these performance standards.
Performance Standards: Face masks are not subject to any regulations. 11 The USA Federal Food and Drug Administration (FDA) classifies face masks as Class II devices. To obtain the necessary approval to sell masks all that a manufacturer need do is satisfy the FDA that any new device is substantially the same as any mask currently available for sale. 21 As ironically noted by the Occupational Health and Safety Agency for Healthcare in BC, “There is no specific requirement to prove that the existing masks are effective and there is no standard test or set of data required supporting the assertion of equivalence. Nor does the FDA conduct or sponsor testing of surgical masks.” 21 Although the FDA recommends two filter efficiency tests; particulate filtration efficiency (PFE) and bacterial filtration efficiency (BFE) it does not stipulate a minimum level of filter performance for these tests. 27 The PFE test is a basis for comparing the efficiency of face masks when exposed to aerosol particle sizes between 0.1 and 5.0 microns. The test does not assess the effectiveness of a mask in preventing the ingress of potentially harmful particles nor can it be used to characterize the protective nature of a mask. 32 The BFE test is a measure of a mask’s ability to provide protection from large particles expelled by the wearer. It does not provide an assessment of a mask’s ability to protect the wearer. 17 Although these tests are conducted under the auspices of the American Society of Testing and Materials (ASTM) and often produce filtration efficiencies in the range of 95-98 %, they are not a measure of a masks ability to protect against respiratory pathogens. Failure to appreciate the limitations of these tests combined with a reliance on the high filtration efficiencies reported by the manufacturers has, according to Healthcare in BC, “created an environment in which health care workers think they are more protected than they actually are.” 21 For dental personnel the protection sought is mainly from treatment induced aerosols.
Dental Aerosols
For approximately 40 years it has been known that dental restorative and especially ultrasonic scaling procedures produce aerosols containing not only blood and saliva but potentially pathogenic organisms. 33 The source of these organisms could be the oral cavities of patients and/or dental unit water lines. 34 Assessing the source and pathogenicity of these organisms has proven elusive as it is extremely difficult to culture bacteria especially anaerobes and viruses from dental aerosols. 34 Although there is no substantiated proof that dental aerosols are an infection control risk, it is a reasonable assumption that if pathogenic microbes are present at the treatment site they will become aerosolized and prone to inhalation by the clinician which a face mask will not prevent. As shown by the study of UK dentists, the inhalation resulted in the formation of appropriate antibodies to respiratory pathogens without overt signs and symptoms of respiratory distress. 14 This occurred whether masks were or were not worn. In a 2008 article, Dr. S. Harrel, of the Baylor College of Dentistry, is of the opinion that because there is a lack of epidemiologically detectable disease from the use of ultrasonic scalers, dental aerosols appear to have a low potential for transmitting disease but should not be ignored as a risk for disease transmission. 34 The most effective measures for reducing disease transmission from dental aerosols are pre-procedural rinses with mouthwashes such as chlorhexidine, large diameter high volume evacuators, and rubber dam whenever possible. 33 Face masks are not useful for this purpose, and Dr. Harrel believes that dental personnel have placed too great a reliance on their efficacy. 34 Perhaps this has occurred because dental regulatory agencies have failed to appreciate the increasing evidence on face mask inadequacies.
The Inadequacies
Between 2004 and 2016 at least a dozen research or review articles have been published on the inadequacies of face masks. 5,6,11,17,19,20,21,25,26,27,28,31 All agree that the poor facial fit and limited filtration characteristics of face masks make them unable to prevent the wearer inhaling airborne particles. In their well-referenced 2011 article on respiratory protection for healthcare workers, Drs. Harriman and Brosseau conclude that, “facemasks will not protect against the inhalation of aerosols.” 11 Following their 2015 literature review, Dr. Zhou and colleagues stated, “There is a lack of substantiated evidence to support claims that facemasks protect either patient or surgeon from infectious contamination.” 25 In the same year Dr. R. MacIntyre noted that randomized controlled trials of facemasks failed to prove their efficacy. 5 In August 2016 responding to a question on the protection from facemasks the Canadian Centre for Occupational Health and Safety replied:
- The filter material of surgical masks does not retain or filter out submicron particles;
- Surgical masks are not designed to eliminate air leakage around the edges;
- Surgical masks do not protect the wearer from inhaling small particles that can remain airborne for long periods of time. 31
In 2015, Dr. Leonie Walker, Principal Researcher of the New Zealand Nurses Organization succinctly described- within a historical context – the inadequacies of facemasks, “Health care workers have long relied heavily on surgical masks to provide protection against influenza and other infections. Yet there are no convincing scientific data that support the effectiveness of masks for respiratory protection. The masks we use are not designed for such purposes, and when tested, they have proved to vary widely in filtration capability, allowing penetration of aerosol particles ranging from four to 90%.” 35
Face masks do not satisfy the criteria for effectiveness as described by Drs. Landefeld and Shojania in their NEJM article, “The Tension between Needing to Improve Care and Knowing How to Do It. 10 The authors declare that, “…recommending or mandating the widespread adoption of interventions to improve quality or safety requires rigorous testing to determine whether, how, and where the intervention is effective…” They stress the critical nature of this concept because, “…a number of widely promulgated interventions are likely to be wholly ineffective, even if they do not harm patients.” 10 A significant inadequacy of face masks is that they were mandated as an intervention based on an assumption rather than on appropriate testing.
Conclusions
The primary reason for mandating the wearing of face masks is to protect dental personnel from airborne pathogens. This review has established that face masks are incapable of providing such a level of protection. Unless the Centers for Disease Control and Prevention, national and provincial dental associations and regulatory agencies publically admit this fact, they will be guilty of perpetuating a myth which will be a disservice to the dental profession and its patients. It would be beneficial if, as a consequence of the review, all present infection control recommendations were subjected to the same rigorous testing as any new clinical intervention. Professional associations and governing bodies must ensure the clinical efficacy of quality improvement procedures prior to them being mandated. It is heartening to know that such a trend is gaining a momentum which might reveal the inadequacies of other long held dental infection control assumptions. Surely, the hallmark of a mature profession is one which permits new evidence to trump established beliefs. In 1910, Dr. C. Chapin, a public health pioneer, summarized this idea by stating, “We should not be ashamed to change our methods; rather, we should be ashamed not to do so.” 36 Until this occurs, as this review has revealed, dentists have nothing to fear by unmasking. OH
Oral Health welcomes this original article.
References
1. Ontario Ministry of Health and Long-term Care. SARS Commission-Spring of Fear: Final Report. Available at: http://www.health.gov.on.ca/english/public/pub/ministry_reports/campbell06/campbell06.html
2. Molinari JA, Nelson P. Face Mask Performance: Are You Protected? Oral Health, March 2016.
3. Diekema D. Controversies in Hospital Infection Prevention, October, 2009.
4. Unmasking the Surgical Mask: Does It Really Work? Medpage Today, Infectious Disease, October, 2009.
5. MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ 2015; 350:h694.
6. Brosseau LM, Jones R. Commentary: Health workers need optimal respiratory protection for Ebola. Center for Infectious Disease Research and Policy. September, 2014.
7. Clinical Habits Die Hard: Nursing Traditions Often Trump Evidence-Based Practice. Infection Control Today, April, 2014.
8. Landman K. Doctors, take off those dirty white coats. National Post, December 7, 2015.
9. Sibert K. Germs and the Pseudoscience of Quality Improvement. California Society of Anesthesiologists, December 8, 2014.
10. Auerbach AD, Landfeld CS, Shojania KG. The Tension between Needing to Improve Care and Knowing How to Do It. NEJM 2007; 357 (6):608-613.
11. Harriman KH, Brosseau LM. Controversy: Respiratory Protection for Healthcare Workers. April, 2011. Available at: http://www.medscape.com/viewarticle/741245_print
12. Bacteria and Viruses Issues. Water Quality Association, 2016. Available at: https://www.wqa.org/Learn-About-Water/Common-Contaminants/Bacteria-Viruses
13. Lechtzin N. Defense Mechanisms of the Respiratory System. Merck Manuals, Kenilworth, USA, 2016
14. Davies KJ, Herbert AM, Westmoreland D. Bagg J. Seroepidemiological study of respiratory virus infections among dental surgeons. Br Dent J. 1994; 176(7):262-265.
15. Shimpo H, Yokoyama E, Tsurumaki K. Causes of death and life expectancies among dentists. Int Dent J 1998; 48(6):563-570.
16. Bureau of Economic Research and Statistics, Mortality of Dentists 1961-1966. JADA 1968; 76(4):831-834.
17. Respirators and Surgical Masks: A Comparison. 3 M Occupational Health and Environment Safety Division. Oct. 2009.
18. Brosseau L. N95 Respirators and Surgical Masks. Centers for Disease Control and Prevention. Oct. 2009.
19. Johnson DF, Druce JD, Birch C, Grayson ML. A Quantitative Assessment of the Efficacy of Surgical and N95 Masks to Filter Influenza Virus in Patients with Acute Influenza Infection. Clin Infect Dis 2009; 49:275-277.
20. Weber A, Willeke K, Marchloni R et al. Aerosol penetration and leakage characteristics of masks used in the health care industry. Am J Inf Cont 1993; 219(4):167-173.
21. Yassi A, Bryce E. Protecting the Faces of Health Care Workers. Occupational Health and Safety Agency for Healthcare in BC, Final Report, April 2004.
22. Bahli ZM. Does Evidence Based Medicine Support The Effectiveness Of Surgical Facemasks In Preventing Postoperative Wound Infections In Elective Surgery. J Ayub Med Coll Abbottabad 2009; 21(2)166-169.
23. Lipp A, Edwards P. Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database Syst Rev 2002(1) CD002929.
24. Lipp A, Edwards P. Disposable surgical face masks: a systematic review. Can Oper Room Nurs J 2005; 23(#):20-38.
25. Zhou Cd, Sivathondan P, Handa A. Unmasking the surgeons: the evidence base behind the use of facemasks in surgery. JR Soc Med 2015; 108(6):223-228.
26. Brosseau L, Jones R. Commentary: Protecting health workers from airborne MERS-CoV- learning from SARS. Center for Infectious Disease Research and Policy May 2014.
27. Oberg T, Brosseau L. Surgical mask filter and fit performance. Am J Infect Control 2008; 36:276-282.
28. Lipp A. The effectiveness of surgical face masks: what the literature shows. Nursing Times 2003; 99(39):22-30.
29. Chen CC, Lehtimaki M, Willeke K. Aerosol penetration through filtering facepieces and respirator cartridges. Am Indus Hyg Assoc J 1992; 53(9):566-574.
30. Chen CC, Willeke K. Characteristics of Face Seal Leakage in Filtering Facepieces. Am Indus Hyg Assoc J 1992; 53(9):533-539.
31. Do surgical masks protect workers? OSH Answers Fact Sheets. Canadian Centre for Occupational health and Safety. Updated August 2016.
32. Standard Test Method for Determining the Initial Efficiency of Materials Used in Medical Face Masks to Penetration by Particulates Using Latex Spheres. American Society of Testing and Materials, Active Standard ASTM F2299/F2299M.
33. Harrel SK. Airborne Spread of Disease-The Implications for Dentistry. CDA J 2004; 32(11); 901-906.
34. Harrel SK. Are Ultrasonic Aerosols an Infection Control Risk? Dimensions of Dental Hygiene 2008; 6(6):20-26.
35. Robinson L. Unmasking the evidence. New Zealand Nurses Organization. May 2015. Available at: https://nznoblog.org.nz/2015/05/15/unmasking-the-evidence
36. Chapin CV. The Sources and Modes of Transmission. New York, NY: John Wiley & Sons; 1910.
The failure to take into account the impact of extreme measures that have become the norm inmany places in the Covid-19 pandemic has been stunning. The destruction of lives and livelihoods in the name of survival will haunt us for decades.
Today’s fear is fueled by four main forces:
1. Mathematical disease modelling – a flexible and highly adaptable tool for prediction, mixing calculations with speculations, often based on
codes that are kept secret and assumptions that are difficult to scrutinize from the outside.
2. Neoliberal policies –systematic disinvestments in public health and medical care that have created fragile systems unable to cope with the crisis.
3. Nervous media reporting – an endless stream of information, obsessed with absolute numbers, exploiting the lack of trust in the healthcare infrastructure and magnifying the fear of collapsing systems.
4. Authoritarian longings – a deep desire for sovereign rule, which derives pleasure from destruction and tries to push the world to the edge of collapse so that it can be rebuilt from the scratch.
The evidence to date suggests that children spread SARS‐CoV‐2 virus relatively rarely and that children are usually infected by symptomatic or pre‐symptomatic adults (in the first 48 h before they become symptomatic). During contact tracing, the China/World Health Organization joint commission recorded no episodes where transmission occurred from a child to an adult. A review of 31 family clusters of COVID‐19 from China, Singapore, the USA, South Korea and Vietnam, found only three (9.7%) clusters had a child as the index case and in all three clusters the child was symptomatic.
Flaxman et al. (Nature, 8 June 2020, https://doi.org/10.1038/s41586-020-2405-7, 2020) infer that non-pharmaceutical interventions conducted by several European countries considerably reduced effective reproduction numbers and saved millions of lives. We show that their method is ill-conceived and that the alleged effects are artefacts. Moreover, we demonstrate that the United Kingdom’s lockdown was both superfluous and ineffective.

Up to 81% of of the population can mount a strong response to COVID-19 without ever having been exposed to it before:
Cross-reactive SARS-CoV-2 T-cell epitopes revealed preexisting T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity
The SARS-CoV-2 pandemic calls for the rapid development of diagnostic, preventive, and therapeutic approaches. CD4+ and CD8+ T cell-mediated immunity is central for control of and protection from viral infections[1-3]. A prerequisite to characterize T-cell immunity, but also for the development of vaccines and immunotherapies, is the identification of the exact viral T-cell epitopes presented on human leukocyte antigens (HLA)[2-8]. This is the first work identifying and characterizing SARS-CoV-2-specific and cross-reactive HLA class I and HLA-DR T-cell epitopes in SARS-CoV-2 convalescents (n = 180) as well as unexposed individuals (n = 185) and confirming their relevance for immunity and COVID-19 disease course. SARS-CoV-2-specific T-cell epitopes enabled detection of post-infectious T-cell immunity, even in seronegative convalescents. Cross-reactive SARS-CoV-2 T-cell epitopes revealed preexisting T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity[9] in SARS-CoV-2 infection[10,11]. Intensity of T-cell responses and recognition rate of T-cell epitopes was significantly higher in the convalescent donors compared to unexposed individuals, suggesting that not only expansion, but also diversity spread of SARS-CoV-2 T-cell responses occur upon active infection. Whereas anti-SARS-CoV-2 antibody levels were associated with severity of symptoms in our SARS-CoV-2 donors, intensity of T-cell responses did not negatively affect COVID-19 severity. Rather, diversity of SARS-CoV-2 T-cell responses was increased in case of mild symptoms of COVID-19, providing evidence that development of immunity requires recognition of multiple SARS-CoV-2 epitopes. Together, the specific and cross-reactive SARS-CoV-2 T-cell epitopes identified in this work enable the identification of heterologous and post-infectious T-cell immunity and facilitate the development of diagnostic, preventive, and therapeutic measures for COVID-19.
The source of bacterial contamination in SMs was the body surface of the surgeons rather than the OR environment. Moreover, we recommend that surgeons should change the mask after each operation, especially those beyond 2 hours. Double-layered SMs or those with excellent filtration function may also be a better alternative.
https://www.sciencedirect.com/science/article/pii/S2214031X18300809
Mask Facts – AAPS
Mask facts from The Association of American Physicians and Surgeons:
- Conclusion: Wearing masks will not reduce SARS-CoV-2.N95 masks protect health care workers, but are not recommended for source control transmission.
- Surgical masks are better than cloth but not very efficient at preventing emissions from infected patients.
- Cloth masks will be ineffective at preventing SARS-CoV-2 transmission, whether worn as source control or as personal protective equipment (PPE).
- Known patients infected with SARS-CoV-2 wore masks and coughed into a Petrie dish. “Both surgical and cotton masks seem to be ineffective in preventing the dissemination of SARS–CoV-2 from the coughs of patients with COVID-19 to the environment and external mask surface.”
- Medical masks offered no protection at all from influenza.
- The wide use of masks by healthy people in the community setting is not supported by current evidence and carries uncertainties and critical risks.
- If you are sick, stay home!
In June 2020, The Office for National Statistics released their Gross domestic product (GDP) report for April 2020. They calculated that GDP fell by 10.4% in the three months to April. This was directly caused by the UK government’s policy of lockdown.
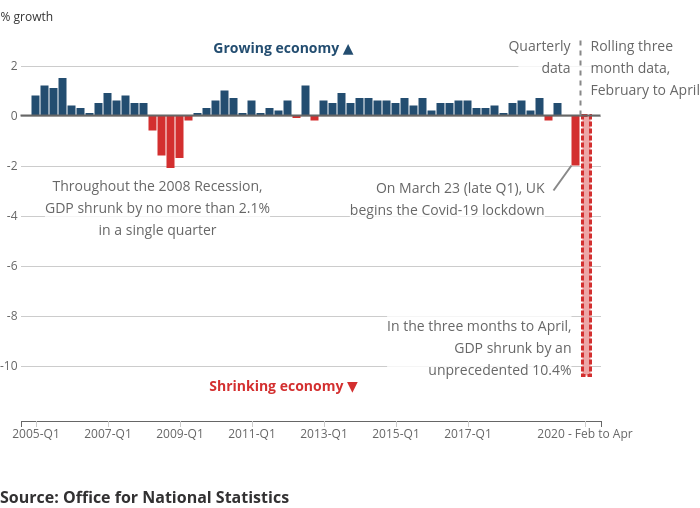
https://www.ons.gov.uk/economy/grossdomesticproductgdp/bulletins/gdpmonthlyestimateuk/april2020
No test gives a 100% accurate result; tests need to be evaluated to determine their sensitivity and specificity, ideally by comparison with a “gold standard.” The lack of such a clear-cut “gold-standard” for covid-19 testing makes evaluation of test accuracy challenging.
A systematic review of the accuracy of covid-19 tests reported false negative rates of between 2% and 29% (equating to sensitivity of 71-98%), based on negative RT-PCR tests which were positive on repeat testing. The use of repeat RT-PCR testing as gold standard is likely to underestimate the true rate of false negatives, as not all patients in the included studies received repeat testing and those with clinically diagnosed covid-19 were not considered as actually having covid-19.
Further evidence and independent validation of covid-19 tests are needed. As current studies show marked variation and are likely to overestimate sensitivity, we will use the lower end of current estimates from systematic reviews, with the approximate numbers of 70% for sensitivity and 95% for specificity for illustrative purposes.
Most Flu Is Asymptomatic
On average, roughly 20% of the unvaccinated had serologic evidence of influenza infection, but up to three quarters of the infected were asymptomatic. The proportions did not vary significantly between seasonal and pandemic influenzas. The pandemic H1N1 strain was associated with less severe symptoms than the seasonal H3N2 strain.
NEJM Journal Watch, 17 March 2014
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(14)70034-7/fulltext
More than 1.6 million Americans have been infected with SARS-CoV-2 and >10 times that number carry antibodies to it. High-risk patients presenting with progressing symptomatic disease have only hospitalization treatment with its high mortality. An outpatient treatment that prevents hospitalization is desperately needed. Two candidate medications have been widely discussed: remdesivir, and hydroxychloroquine+azithromycin. Remdesivir has shown mild effectiveness in hospitalized inpatients, but no trials have been registered in outpatients. Hydroxychloroquine+azithromycin has been widely misrepresented in both clinical reports and public media, and outpatient trials results are not expected until September. Early outpatient illness is very different than later hospitalized florid disease and the treatments differ. Evidence about use of hydroxychloroquine alone, or of hydroxychloroquine+azithromycin in inpatients, is irrelevant concerning efficacy of the pair in early high-risk outpatient disease. Five studies, including two controlled clinical trials, have demonstrated significant major outpatient treatment efficacy. Hydroxychloroquine+azithromycin has been used as standard-of-care in more than 300,000 older adults with multicomorbidities, with estimated proportion diagnosed with cardiac arrhythmias attributable to the medications 47/100,000 users, of which estimated mortality is <20%, 9/100,000 users, compared to the 10,000 Americans now dying each week. These medications need to be widely available and promoted immediately for physicians to prescribe.
https://academic.oup.com/aje/advance-article/doi/10.1093/aje/kwaa093/5847586
Estimates of asymptomatic rate and transmission rate are vital parameters for modelling studies. Our estimates of the proportion of asymptomatic cases and their transmission rates suggest that asymptomatic spread is unlikely to be a major driver of clusters or community transmission of infection, but the extent for pre-symptomatic and minor symptomatic transmission remains unknown. Other unknowns include whether there is a difference in age (particularly children vs adults), sex and underlying comorbidities that differentiate asymptomatic from pre-symptomatic cases; development of long-term immunity; and whether asymptomatic cases take longer to develop active disease or remain silent.
https://www.medrxiv.org/content/10.1101/2020.05.10.20097543v2.full
Asymptomatic SARS-CoV-2 infection is common and can be detected by analysis of saliva or NTS. NTS viral loads fall faster in asymptomatic individuals, but they appear able to transmit the virus to others.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa711/5851471