There were 3 influenza pandemics in the 20th century, and there has been 1 so far in the 21st century. Local, national, and international health authorities regularly update their plans for mitigating the next influenza pandemic in light of the latest available evidence on the effectiveness of various control measures in reducing transmission. Here, we review the evidence base on the effectiveness of nonpharmaceutical personal protective measures and environmental hygiene measures in nonhealthcare settings and discuss their potential inclusion in pandemic plans. Although mechanistic studies support the potential effect of hand hygiene or face masks, evidence from 14 randomized controlled trials of these measures did not support a substantial effect on transmission of laboratory-confirmed influenza. We similarly found limited evidence on the effectiveness of improved hygiene and environmental cleaning. We identified several major knowledge gaps requiring further research, most fundamentally an improved characterization of the modes of person-to-person transmission.
EvidenceNotFear
Browse the articles related to this topic below.
Join our community on Guilded.
Note: This article, published on 16 October 2016, originally appeared in the Oral Health website. It was removed sometime after the end of June 2020 with no explanation other than, it being ‘no longer relevant in our current climate.’
The science behind face masks has not changed considerably in the past few months so we can only guess about what ‘no longer relevant’ means.
While you can find a capture at archive.org, we have saved a copy here to protect against censorship and for easy sharing.
Yesterday’s Scientific Dogma is Today’s Discarded Fable
Introduction
The above quotation is ascribed to Justice Archie Campbell author of Canada’s SARS Commission Final Report. 1 It is a stark reminder that scientific knowledge is constantly changing as new discoveries contradict established beliefs. For at least three decades a face mask has been deemed an essential component of the personal protective equipment worn by dental personnel. A current article, “Face Mask Performance: Are You Protected” gives the impression that masks are capable of providing an acceptable level of protection from airborne pathogens. 2 Studies of recent diseases such as Severe Acute Respiratory Syndrome (SARS), Middle Eastern Respiratory Syndrome (MERS) and the Ebola Crisis combined with those of seasonal influenza and drug resistant tuberculosis have promoted a better understanding of how respiratory diseases are transmitted. Concurrently, with this appreciation, there have been a number of clinical investigations into the efficacy of protective devices such as face masks. This article will describe how the findings of such studies lead to a rethinking of the benefits of wearing a mask during the practice of dentistry. It will begin by describing new concepts relating to infection control especially personal protective equipment (PPE).
Trends in Infection Control
For the past three decades there has been minimal opposition to what have become seemingly established and accepted infection control recommendations. In 2009, infection control specialist Dr. D. Diekema questioned the validity of these by asking what actual, front-line hospital-based infection control experiences were available to such authoritative organization as the Centers for Disease Control and Prevention (CDC), the Occupational Safety and Health Association (OSHA) and the National Institute for Occupational Safety and Health (NIOSH). 3 In the same year, while commenting on guidelines for face masks, Dr. M. Rupp of the Society for Healthcare Epidemiology of America noted that some of the practices relating to infection control that have been in place for decades, ”haven’t been subjected to the same strenuous investigation that, for instance, a new medicine might be subjected.” 4 He opined that perhaps it is the relative cheapness and apparent safety of face masks that has prevented them from undergoing the extensive studies that should be required for any quality improvement device. 4 More recently, Dr. R. MacIntyre, a prolific investigator of face masks, has forcefully stated that the historical reliance on theoretical assumptions for recommending PPEs should be replaced by rigorously acquired clinical data. 5 She noted that most studies on face masks have been based on laboratory simulated tests which quite simply have limited clinical applicability as they cannot account for such human factors as compliance, coughing and talking. 5
Covering the nose and mouth for infection control started in the early 1900s when the German physician Carl Flugge discovered that exhaled droplets could transmit tuberculosis. 4 The science regarding the aerosol transmission of infectious diseases has, for years, been based on what is now appreciated to be “very outmoded research and an overly simplistic interpretation of the data.” 6 Modern studies are employing sensitive instruments and interpretative techniques to better understand the size and distribution of potentially infectious aerosol particles. 6 Such knowledge is paramount to appreciating the limitations of face masks. Nevertheless, it is the historical understanding of droplet and airborne transmission that has driven the longstanding and continuing tradition of mask wearing among health professionals. In 2014, the nursing profession was implored to “stop using practice interventions that are based on tradition” but instead adopt protocols that are based on critical evaluations of the available evidence. 7
A December 2015 article in the National Post seems to ascribe to Dr. Gardam, Director of Infection Prevention and Control, Toronto University Health Network the quote, “I need to choose which stupid, arbitrary infection control rules I’m going to push.” 8 In a communication with the author, Dr. Gardam explained that this was not a personal belief but that it did reflect the views of some infection control practitioners. In her 2014 article, “Germs and the Pseudoscience of Quality Improvement”, Dr. K Sibert, an anaesthetist with an interest in infection control, is of the opinion that many infection control rules are indeed arbitrary, not justified by the available evidence or subjected to controlled follow-up studies, but are devised, often under pressure, to give the appearance of doing something. 9
The above illustrate the developing concerns that many infection control measures have been adopted with minimal supporting evidence. To address this fault, the authors of a 2007 New England Journal of Medicine (NEJM) article eloquently argue that all safety and quality improvement recommendations must be subjected to the same rigorous testing as would any new clinical intervention. 10 Dr. R. MacIntyre, a proponent of this trend in infection control, has used her research findings to boldly state that, “it would not seem justifiable to ask healthcare workers to wear surgical masks.” 4 To understand this conclusion it is necessary to appreciate the current concepts relating to airborne transmissions.
Airborne Transmissions
Early studies of airborne transmissions were hampered by the fact that the investigators were not able to detect small particles (less than 5 microns) near an infectious person. 6 Thus, they assumed that it was the exposure of the face, eyes and nose to large particles (greater than 5 microns) or “droplets” that transmitted the respiratory condition to a person in close proximity to the host. 6 This became known as “droplet infection”, and 5 microns or greater became established as the size of large particles and the traditional belief that such particles could, in theory, be trapped by a face mask. 5 The early researchers concluded that since only large particles were detected near an infectious person any small particles would be transmitted via air currents, dispersed over long distances, remain infective over time and might be inhaled by persons who never had any close contact with the host. 11 This became known as “airborne transmission” against which a face mask would be of little use. 5
Through the use of highly sensitive instruments it is now appreciated that the aerosols transmitted from the respiratory tract due to coughing, sneezing, talking, exhalation and certain medical and dental procedures produce respiratory particles that range from the very small (less than 5 microns) to the very large (greater than a 100 microns) and that all of these particles are capable of being inhaled by persons close to the source. 6, 11 This means that respiratory aerosols potentially contain bacteria averaging in size from 1-10 microns and viruses ranging in size from 0.004 to 0.1 microns. 12 It is also acknowledged that upon their emission large “droplets” will undergo evaporation producing a concentration of readily inhalable small particles surrounding the aerosol source. 6
The historical terms “droplet infection” and “airborne transmission” defined the routes of infection based on particle size. Current knowledge suggests that these are redundant descriptions since aerosols contain a wide distribution of particle sizes and that they ought to be replaced by the term, “aerosol transmissible.” 4, 5 Aerosol transmission has been defined as “person –to – person transmission of pathogens through air by means of inhalation of infectious particles.” 26 In addition, it is appreciated that the physics associated with the production of the aerosols imparts energy to microbial suspensions facilitating their inhalation. 11
Traditionally face masks have been recommended to protect the mouth and nose from the “droplet” route of infection, presumably because they will prevent the inhalation of relatively large particles. 11 Their efficacy must be re-examined in light of the fact that aerosols contain particles many times smaller than 5 microns. Prior to this examination, it is pertinent to review the defence mechanism of the respiratory tract.
Respiratory System Defences
Comprehensive details on the defence mechanisms of the respiratory tract will not be discussed. Instead readers are reminded that; coughing, sneezing, nasal hairs, respiratory tract cilia, mucous producing lining cells and the phagocytic activity of alveolar macrophages provide protection against inhaled foreign bodies including fungi, bacteria and viruses. 13 Indeed, the pathogen laden aerosols produced by everyday talking and eating would have the potential to cause significant disease if it were not for these effective respiratory tract defences.
These defences contradict the recently published belief that dentally produced aerosols, “enter unprotected bronchioles and alveoli.” 2 A pertinent demonstration of the respiratory tract’s ability to resist disease is the finding that- compared to controls- dentists had significantly elevated levels of antibodies to influenza A and B and the respiratory syncytial virus. 14 Thus, while dentists had greater than normal exposure to these aerosol transmissible pathogens, their potential to cause disease was resisted by respiratory immunologic responses. Interestingly, the wearing of masks and eye glasses did not lessen the production of antibodies, thus reducing their significance as personal protective barriers. 14 Another example of the effectiveness of respiratory defences is that although exposed to more aerosol transmissible pathogens than the general population, Tokyo dentists have a significantly lower risk of dying from pneumonia and bronchitis. 15 The ability of a face mask to prevent the infectious risk potentially inherent in sprays of blood and saliva reaching the wearers mouth and nose is questionable since, before the advent of mask use, dentists were no more likely to die of infectious diseases than the general population. 16
The respiratory tract has efficient defence mechanisms. Unless face masks have the ability to either enhance or lessen the need for such natural defences, their use as protection against airborne pathogens must be questioned.
Face Masks
History: Cloth or cotton gauze masks have been used since the late 19th century to protect sterile fields from spit and mucous generated by the wearer. 5,17,18 A secondary function was to protect the mouth and nose of the wearer from the sprays and splashes of blood and body fluids created during surgery. 17 As noted above, in the early 20th century masks were used to trap infectious “droplets” expelled by the wearer thus possibly reducing disease transmission to others. 18 Since the mid-20th century until to-day, face masks have been increasingly used for entirely the opposite function: that is to prevent the wearer from inhaling respiratory pathogens. 5,20,21 Indeed, most current dental infection control recommendations insist that a face mask be worn, “as a key component of personal protection against airborne pathogens”. 2
Literature reviews have confirmed that wearing a mask during surgery has no impact whatsoever on wound infection rates during clean surgery. 22,23,24,25,26 A recent 2014 report states categorically that no clinical trials have ever shown that wearing a mask prevents contamination of surgical sites. 26 With their original purpose being highly questionable it should be no surprise that the ability of face masks to act as respiratory protective devices is now the subject of intense scrutiny. 27 Appreciating the reasons for this, requires an understanding of the structure, fit and filtering capacity of face masks.
Structure and Fit: Disposable face masks usually consist of three to four layers of flat non-woven mats of fine fibres separated by one or two polypropylene barrier layers which act as filters capable of trapping material greater than 1 micron in diameter. 18,24,28 Masks are placed over the nose and mouth and secured by straps usually placed behind the head and neck. 21 No matter how well a mask conforms to the shape of a person’s face, it is not designed to create an air tight seal around the face. Masks will always fit fairly loosely with considerable gaps along the cheeks, around the bridge of the nose and along the bottom edge of the mask below the chin. 21 These gaps do not provide adequate protection as they permit the passage of air and aerosols when the wearer inhales. 11,17 It is important to appreciate that if masks contained filters capable of trapping viruses, the peripheral gaps around the masks would continue to permit the inhalation of unfiltered air and aerosols. 11
Filtering Capacity: The filters in masks do not act as sieves by trapping particles greater than a specific size while allowing smaller particles to pass through. 18 Instead the dynamics of aerosolized particles and their molecular attraction to filter fibres are such that at a certain range of sizes both large and small particles will penetrate through a face mask. 18 Accordingly, it should be no surprise that a study of eight brands of face masks found that they did not filter out 20-100% of particles varying in size from 0.1 to 4.0 microns. 21 Another investigation showed penetration ranges from 5-100% when masks were challenged with relatively large 1.0 micron particles. 29 A further study found that masks were incapable of filtering out 80-85% of particles varying in size from 0.3 to 2.0 microns. 30 A 2008 investigation identified the poor filtering performance of dental masks. 27 It should be concluded from these and similar studies that the filter material of face masks does not retain or filter out viruses or other submicron particles. 11,31 When this understanding is combined with the poor fit of masks, it is readily appreciated that neither the filter performance nor the facial fit characteristics of face masks qualify them as being devices which protect against respiratory infections. 27 Despite this determination the performance of masks against certain criteria has been used to justify their effectiveness.2 Accordingly, it is appropriate to review the limitations of these performance standards.
Performance Standards: Face masks are not subject to any regulations. 11 The USA Federal Food and Drug Administration (FDA) classifies face masks as Class II devices. To obtain the necessary approval to sell masks all that a manufacturer need do is satisfy the FDA that any new device is substantially the same as any mask currently available for sale. 21 As ironically noted by the Occupational Health and Safety Agency for Healthcare in BC, “There is no specific requirement to prove that the existing masks are effective and there is no standard test or set of data required supporting the assertion of equivalence. Nor does the FDA conduct or sponsor testing of surgical masks.” 21 Although the FDA recommends two filter efficiency tests; particulate filtration efficiency (PFE) and bacterial filtration efficiency (BFE) it does not stipulate a minimum level of filter performance for these tests. 27 The PFE test is a basis for comparing the efficiency of face masks when exposed to aerosol particle sizes between 0.1 and 5.0 microns. The test does not assess the effectiveness of a mask in preventing the ingress of potentially harmful particles nor can it be used to characterize the protective nature of a mask. 32 The BFE test is a measure of a mask’s ability to provide protection from large particles expelled by the wearer. It does not provide an assessment of a mask’s ability to protect the wearer. 17 Although these tests are conducted under the auspices of the American Society of Testing and Materials (ASTM) and often produce filtration efficiencies in the range of 95-98 %, they are not a measure of a masks ability to protect against respiratory pathogens. Failure to appreciate the limitations of these tests combined with a reliance on the high filtration efficiencies reported by the manufacturers has, according to Healthcare in BC, “created an environment in which health care workers think they are more protected than they actually are.” 21 For dental personnel the protection sought is mainly from treatment induced aerosols.
Dental Aerosols
For approximately 40 years it has been known that dental restorative and especially ultrasonic scaling procedures produce aerosols containing not only blood and saliva but potentially pathogenic organisms. 33 The source of these organisms could be the oral cavities of patients and/or dental unit water lines. 34 Assessing the source and pathogenicity of these organisms has proven elusive as it is extremely difficult to culture bacteria especially anaerobes and viruses from dental aerosols. 34 Although there is no substantiated proof that dental aerosols are an infection control risk, it is a reasonable assumption that if pathogenic microbes are present at the treatment site they will become aerosolized and prone to inhalation by the clinician which a face mask will not prevent. As shown by the study of UK dentists, the inhalation resulted in the formation of appropriate antibodies to respiratory pathogens without overt signs and symptoms of respiratory distress. 14 This occurred whether masks were or were not worn. In a 2008 article, Dr. S. Harrel, of the Baylor College of Dentistry, is of the opinion that because there is a lack of epidemiologically detectable disease from the use of ultrasonic scalers, dental aerosols appear to have a low potential for transmitting disease but should not be ignored as a risk for disease transmission. 34 The most effective measures for reducing disease transmission from dental aerosols are pre-procedural rinses with mouthwashes such as chlorhexidine, large diameter high volume evacuators, and rubber dam whenever possible. 33 Face masks are not useful for this purpose, and Dr. Harrel believes that dental personnel have placed too great a reliance on their efficacy. 34 Perhaps this has occurred because dental regulatory agencies have failed to appreciate the increasing evidence on face mask inadequacies.
The Inadequacies
Between 2004 and 2016 at least a dozen research or review articles have been published on the inadequacies of face masks. 5,6,11,17,19,20,21,25,26,27,28,31 All agree that the poor facial fit and limited filtration characteristics of face masks make them unable to prevent the wearer inhaling airborne particles. In their well-referenced 2011 article on respiratory protection for healthcare workers, Drs. Harriman and Brosseau conclude that, “facemasks will not protect against the inhalation of aerosols.” 11 Following their 2015 literature review, Dr. Zhou and colleagues stated, “There is a lack of substantiated evidence to support claims that facemasks protect either patient or surgeon from infectious contamination.” 25 In the same year Dr. R. MacIntyre noted that randomized controlled trials of facemasks failed to prove their efficacy. 5 In August 2016 responding to a question on the protection from facemasks the Canadian Centre for Occupational Health and Safety replied:
- The filter material of surgical masks does not retain or filter out submicron particles;
- Surgical masks are not designed to eliminate air leakage around the edges;
- Surgical masks do not protect the wearer from inhaling small particles that can remain airborne for long periods of time. 31
In 2015, Dr. Leonie Walker, Principal Researcher of the New Zealand Nurses Organization succinctly described- within a historical context – the inadequacies of facemasks, “Health care workers have long relied heavily on surgical masks to provide protection against influenza and other infections. Yet there are no convincing scientific data that support the effectiveness of masks for respiratory protection. The masks we use are not designed for such purposes, and when tested, they have proved to vary widely in filtration capability, allowing penetration of aerosol particles ranging from four to 90%.” 35
Face masks do not satisfy the criteria for effectiveness as described by Drs. Landefeld and Shojania in their NEJM article, “The Tension between Needing to Improve Care and Knowing How to Do It. 10 The authors declare that, “…recommending or mandating the widespread adoption of interventions to improve quality or safety requires rigorous testing to determine whether, how, and where the intervention is effective…” They stress the critical nature of this concept because, “…a number of widely promulgated interventions are likely to be wholly ineffective, even if they do not harm patients.” 10 A significant inadequacy of face masks is that they were mandated as an intervention based on an assumption rather than on appropriate testing.
Conclusions
The primary reason for mandating the wearing of face masks is to protect dental personnel from airborne pathogens. This review has established that face masks are incapable of providing such a level of protection. Unless the Centers for Disease Control and Prevention, national and provincial dental associations and regulatory agencies publically admit this fact, they will be guilty of perpetuating a myth which will be a disservice to the dental profession and its patients. It would be beneficial if, as a consequence of the review, all present infection control recommendations were subjected to the same rigorous testing as any new clinical intervention. Professional associations and governing bodies must ensure the clinical efficacy of quality improvement procedures prior to them being mandated. It is heartening to know that such a trend is gaining a momentum which might reveal the inadequacies of other long held dental infection control assumptions. Surely, the hallmark of a mature profession is one which permits new evidence to trump established beliefs. In 1910, Dr. C. Chapin, a public health pioneer, summarized this idea by stating, “We should not be ashamed to change our methods; rather, we should be ashamed not to do so.” 36 Until this occurs, as this review has revealed, dentists have nothing to fear by unmasking. OH
Oral Health welcomes this original article.
References
1. Ontario Ministry of Health and Long-term Care. SARS Commission-Spring of Fear: Final Report. Available at: http://www.health.gov.on.ca/english/public/pub/ministry_reports/campbell06/campbell06.html
2. Molinari JA, Nelson P. Face Mask Performance: Are You Protected? Oral Health, March 2016.
3. Diekema D. Controversies in Hospital Infection Prevention, October, 2009.
4. Unmasking the Surgical Mask: Does It Really Work? Medpage Today, Infectious Disease, October, 2009.
5. MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ 2015; 350:h694.
6. Brosseau LM, Jones R. Commentary: Health workers need optimal respiratory protection for Ebola. Center for Infectious Disease Research and Policy. September, 2014.
7. Clinical Habits Die Hard: Nursing Traditions Often Trump Evidence-Based Practice. Infection Control Today, April, 2014.
8. Landman K. Doctors, take off those dirty white coats. National Post, December 7, 2015.
9. Sibert K. Germs and the Pseudoscience of Quality Improvement. California Society of Anesthesiologists, December 8, 2014.
10. Auerbach AD, Landfeld CS, Shojania KG. The Tension between Needing to Improve Care and Knowing How to Do It. NEJM 2007; 357 (6):608-613.
11. Harriman KH, Brosseau LM. Controversy: Respiratory Protection for Healthcare Workers. April, 2011. Available at: http://www.medscape.com/viewarticle/741245_print
12. Bacteria and Viruses Issues. Water Quality Association, 2016. Available at: https://www.wqa.org/Learn-About-Water/Common-Contaminants/Bacteria-Viruses
13. Lechtzin N. Defense Mechanisms of the Respiratory System. Merck Manuals, Kenilworth, USA, 2016
14. Davies KJ, Herbert AM, Westmoreland D. Bagg J. Seroepidemiological study of respiratory virus infections among dental surgeons. Br Dent J. 1994; 176(7):262-265.
15. Shimpo H, Yokoyama E, Tsurumaki K. Causes of death and life expectancies among dentists. Int Dent J 1998; 48(6):563-570.
16. Bureau of Economic Research and Statistics, Mortality of Dentists 1961-1966. JADA 1968; 76(4):831-834.
17. Respirators and Surgical Masks: A Comparison. 3 M Occupational Health and Environment Safety Division. Oct. 2009.
18. Brosseau L. N95 Respirators and Surgical Masks. Centers for Disease Control and Prevention. Oct. 2009.
19. Johnson DF, Druce JD, Birch C, Grayson ML. A Quantitative Assessment of the Efficacy of Surgical and N95 Masks to Filter Influenza Virus in Patients with Acute Influenza Infection. Clin Infect Dis 2009; 49:275-277.
20. Weber A, Willeke K, Marchloni R et al. Aerosol penetration and leakage characteristics of masks used in the health care industry. Am J Inf Cont 1993; 219(4):167-173.
21. Yassi A, Bryce E. Protecting the Faces of Health Care Workers. Occupational Health and Safety Agency for Healthcare in BC, Final Report, April 2004.
22. Bahli ZM. Does Evidence Based Medicine Support The Effectiveness Of Surgical Facemasks In Preventing Postoperative Wound Infections In Elective Surgery. J Ayub Med Coll Abbottabad 2009; 21(2)166-169.
23. Lipp A, Edwards P. Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database Syst Rev 2002(1) CD002929.
24. Lipp A, Edwards P. Disposable surgical face masks: a systematic review. Can Oper Room Nurs J 2005; 23(#):20-38.
25. Zhou Cd, Sivathondan P, Handa A. Unmasking the surgeons: the evidence base behind the use of facemasks in surgery. JR Soc Med 2015; 108(6):223-228.
26. Brosseau L, Jones R. Commentary: Protecting health workers from airborne MERS-CoV- learning from SARS. Center for Infectious Disease Research and Policy May 2014.
27. Oberg T, Brosseau L. Surgical mask filter and fit performance. Am J Infect Control 2008; 36:276-282.
28. Lipp A. The effectiveness of surgical face masks: what the literature shows. Nursing Times 2003; 99(39):22-30.
29. Chen CC, Lehtimaki M, Willeke K. Aerosol penetration through filtering facepieces and respirator cartridges. Am Indus Hyg Assoc J 1992; 53(9):566-574.
30. Chen CC, Willeke K. Characteristics of Face Seal Leakage in Filtering Facepieces. Am Indus Hyg Assoc J 1992; 53(9):533-539.
31. Do surgical masks protect workers? OSH Answers Fact Sheets. Canadian Centre for Occupational health and Safety. Updated August 2016.
32. Standard Test Method for Determining the Initial Efficiency of Materials Used in Medical Face Masks to Penetration by Particulates Using Latex Spheres. American Society of Testing and Materials, Active Standard ASTM F2299/F2299M.
33. Harrel SK. Airborne Spread of Disease-The Implications for Dentistry. CDA J 2004; 32(11); 901-906.
34. Harrel SK. Are Ultrasonic Aerosols an Infection Control Risk? Dimensions of Dental Hygiene 2008; 6(6):20-26.
35. Robinson L. Unmasking the evidence. New Zealand Nurses Organization. May 2015. Available at: https://nznoblog.org.nz/2015/05/15/unmasking-the-evidence
36. Chapin CV. The Sources and Modes of Transmission. New York, NY: John Wiley & Sons; 1910.
A coronavirus vaccine professor at Oxford University says there is now ‘little chance’ of proving if it works due to low transmission rates in the UK.
Professor Sarah Gilbert, leading the University of Oxford vaccine trial, said that when Covid-19 transmission was high, lockdown was imposed to bring the rate down.
But since then rates have dropped, and the trial relies on a sufficient number of volunteers to have been exposed to the virus to see whether a vaccine protects them or not.
https://www.mirror.co.uk/news/uk-news/vaccine-professor-oxford-university-says-22241101
Scientists at Institut Pasteur studied 1,340 people in Crepy-en-Valois, a town northeast of Paris that suffered an outbreak in February and March, including 510 students from six primary schools. They found three probable cases among kids that didn’t lead to more infections among other pupils or teachers.
The study confirms that children appear to show fewer telltale symptoms than adults and be less contagious, providing a justification for school reopenings in countries from Denmark to Switzerland. The researchers found that 61% of the parents of infected kids had the coronavirus, compared with about 7% of parents of healthy ones, suggesting it was the parents who had infected their offspring rather than the other way around.
It is official. No 10 is too entangled in lockdown spin to do what it takes to save Britain. For the sake of our ailing economy, political clarity, and basic scientific honesty, this was Boris Johnson’s moment to declare to the nation that the overwhelming evidence suggests lockdown was a mistake – and we must never lock down again.
Professor Matteo Bassetti said he is convinced the virus is ‘changing in severity’ and patients are now surviving infections that would have killed them before.
And if the virus’s weakening is true, Covid-19 could even disappear without a for a vaccine by becoming so weak it dies out on its own, he claimed.
Professor Bassetti suggests this could be because of a genetic mutation in the virus making it less lethal, because of improved treatments, or because people are not getting infected with such large doses because of social distancing.
But other scientists have hit back at the claims in the past and said there is no scientific evidence that the virus has changed at all.
At the start of June, in response to Professor Bassetti’s claim, Dr Angela Rasmussen, from Columbia University, tweeted: ‘There is no evidence that the virus is losing potency anywhere.’
NHS doctors are prematurely ending the lives of thousands of elderly hospital patients because they are difficult to manage or to free up beds, a senior consultant claimed yesterday.
Professor Patrick Pullicino said doctors had turned the use of a controversial ‘death pathway’ into the equivalent of euthanasia of the elderly.
He claimed there was often a lack of clear evidence for initiating the Liverpool Care Pathway, a method of looking after terminally ill patients that is used in hospitals across the country.
Professor Pullicino claimed that far too often elderly patients who could live longer are placed on the LCP and it had now become an ‘assisted death pathway rather than a care pathway’.
The failure to take into account the impact of extreme measures that have become the norm inmany places in the Covid-19 pandemic has been stunning. The destruction of lives and livelihoods in the name of survival will haunt us for decades.
Today’s fear is fueled by four main forces:
1. Mathematical disease modelling – a flexible and highly adaptable tool for prediction, mixing calculations with speculations, often based on
codes that are kept secret and assumptions that are difficult to scrutinize from the outside.
2. Neoliberal policies –systematic disinvestments in public health and medical care that have created fragile systems unable to cope with the crisis.
3. Nervous media reporting – an endless stream of information, obsessed with absolute numbers, exploiting the lack of trust in the healthcare infrastructure and magnifying the fear of collapsing systems.
4. Authoritarian longings – a deep desire for sovereign rule, which derives pleasure from destruction and tries to push the world to the edge of collapse so that it can be rebuilt from the scratch.
The evidence to date suggests that children spread SARS‐CoV‐2 virus relatively rarely and that children are usually infected by symptomatic or pre‐symptomatic adults (in the first 48 h before they become symptomatic). During contact tracing, the China/World Health Organization joint commission recorded no episodes where transmission occurred from a child to an adult. A review of 31 family clusters of COVID‐19 from China, Singapore, the USA, South Korea and Vietnam, found only three (9.7%) clusters had a child as the index case and in all three clusters the child was symptomatic.
Flaxman et al. (Nature, 8 June 2020, https://doi.org/10.1038/s41586-020-2405-7, 2020) infer that non-pharmaceutical interventions conducted by several European countries considerably reduced effective reproduction numbers and saved millions of lives. We show that their method is ill-conceived and that the alleged effects are artefacts. Moreover, we demonstrate that the United Kingdom’s lockdown was both superfluous and ineffective.

No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.
Likewise, no study exists that shows a benefit from a broad policy to wear masks in public.
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Regarding the aerosol mechanism of infectious disease transmission:
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
[I]f anything gets through (and it always does, irrespective of the mask), then you are going to be infected. Masks cannot possibly work. It is not surprising, therefore, that no bias-free study has ever found a benefit from wearing a mask or respirator in this application.
Regarding minimal infective dose:
- Most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- It is believed that a single virion can be enough to induce illness in the host
- The 50-percent probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- There are typically 10 to 3rd power − 10 to 7th power virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- The 50-percent probability MID easily fits into a single (one) aerolized droplet
- For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans,“we estimate that after a delay of ~6 h, infected cells begin producing influenza virus and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90 percent of infected cell are significantly impacted, rather than simply surviving unharmed.
Regarding tests for a wide-scale mask-wearing policy:
- Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
- Mask compliance and mask adjustment habits would be unknown.
- Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
- The results would not be transferable, because of differing cultural habits.
- Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
- Monitoring and compliance measurement are near-impossible, and subject to large errors.
- Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
- Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
- Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Unanswered questions about mask-wearing:
- Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
- Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
- Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
- What are the dangers of bacterial growth on a used and loaded mask?
- How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
- What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
- Are there negative social consequences to a masked society?
- Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
- What are the environmental consequences of mask manufacturing and disposal?
- Do the masks shed fibers or substances that are harmful when inhaled?
Up to 81% of of the population can mount a strong response to COVID-19 without ever having been exposed to it before:
Cross-reactive SARS-CoV-2 T-cell epitopes revealed preexisting T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity
The SARS-CoV-2 pandemic calls for the rapid development of diagnostic, preventive, and therapeutic approaches. CD4+ and CD8+ T cell-mediated immunity is central for control of and protection from viral infections[1-3]. A prerequisite to characterize T-cell immunity, but also for the development of vaccines and immunotherapies, is the identification of the exact viral T-cell epitopes presented on human leukocyte antigens (HLA)[2-8]. This is the first work identifying and characterizing SARS-CoV-2-specific and cross-reactive HLA class I and HLA-DR T-cell epitopes in SARS-CoV-2 convalescents (n = 180) as well as unexposed individuals (n = 185) and confirming their relevance for immunity and COVID-19 disease course. SARS-CoV-2-specific T-cell epitopes enabled detection of post-infectious T-cell immunity, even in seronegative convalescents. Cross-reactive SARS-CoV-2 T-cell epitopes revealed preexisting T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity[9] in SARS-CoV-2 infection[10,11]. Intensity of T-cell responses and recognition rate of T-cell epitopes was significantly higher in the convalescent donors compared to unexposed individuals, suggesting that not only expansion, but also diversity spread of SARS-CoV-2 T-cell responses occur upon active infection. Whereas anti-SARS-CoV-2 antibody levels were associated with severity of symptoms in our SARS-CoV-2 donors, intensity of T-cell responses did not negatively affect COVID-19 severity. Rather, diversity of SARS-CoV-2 T-cell responses was increased in case of mild symptoms of COVID-19, providing evidence that development of immunity requires recognition of multiple SARS-CoV-2 epitopes. Together, the specific and cross-reactive SARS-CoV-2 T-cell epitopes identified in this work enable the identification of heterologous and post-infectious T-cell immunity and facilitate the development of diagnostic, preventive, and therapeutic measures for COVID-19.
According to the president, the World Bank has showed interest in Belarus’ coronavirus response practices. “It is ready to fund us ten times more than it offered initially as a token of commendation for our efficient fight against this virus. The World Bank has even asked the Healthcare Ministry to share the experience. Meanwhile, the IMF continues to demand from us quarantine measures, isolation, a curfew. This is nonsense. We will not dance to anyone’s tune,” said the president.
Italian scientists say sewage water from two cities contained coronavirus traces in December, long before the country’s first confirmed cases.
The National Institute of Health (ISS) said water from Milan and Turin showed genetic virus traces on 18 December.
It adds to evidence from other countries that the virus may have been circulating much earlier than thought.
The source of bacterial contamination in SMs was the body surface of the surgeons rather than the OR environment. Moreover, we recommend that surgeons should change the mask after each operation, especially those beyond 2 hours. Double-layered SMs or those with excellent filtration function may also be a better alternative.
https://www.sciencedirect.com/science/article/pii/S2214031X18300809
By now, we ought to be seeing some evidence of increasing Covid-19 cases from the mass protests. The fact we are not raises very serious doubts about the coronavirus lockdowns and other non-pharmaceutical interventions, many of which are still ongoing.
…The third explanatory hypothesis is that we have vastly overestimated certain risks from Covid-19, limiting fundamental civil liberties of law-abiding citizens and getting it wrong. It finally took unsanctioned mass protests to prove this point.
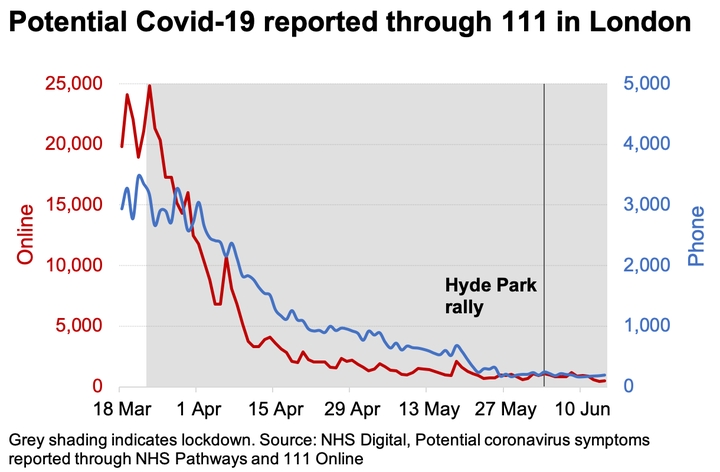
https://www.spectator.co.uk/article/why-haven-t-we-seen-a-post-protest-covid-spike-
Cleveland Clinic CEO and Mayo Clinic President say the response to COVID-19 could be as big a disaster as the virus itself.
“The true cost of this epidemic will not be measured in dollars; it will be measured in human lives and human suffering. In the case of cancer alone, our calculations show we can expect a quarter of a million additional preventable deaths annually if normal care does not resume,” they wrote.
https://www.nytimes.com/2020/06/09/opinion/coronavirus-hospitals-deaths.html
Researchers found school closures had little effect on preventing coronavirus transmission compared to that of the flu.
Under-20s are half as likely to catch COVID-19 as over-20s, making school closures less effective at stopping the spread of the virus, a new scientific study has found.
Researchers at the London School of Hygiene and Tropical Medicine found that susceptibility to the coronavirus was low for younger people, before increasing around the age of 20.
The two-metre social distancing guidance is “not an absolute rule” and “can only remain in place as long as there is consent”, a cabinet minister has said.
Jacob Rees-Mogg, the leader of the Commons, said the measure was “guidance rather than an absolute rule that will be enforced by a policeman”.
Speaking on his fortnightly Moggcast on the Conservative Home website, he added: “My view of all the restrictions is that they have happened by consent rather than compulsion.”
After years of a near jobs miracle that saw record numbers in employment, Covid-19 is taking a brutal toll.
Figures from the ONS today show that the number of staff on UK payrolls fell by 612,000 between March and May.
Claimant unemployment is already up by 1.6 million since March to 2.8 million. In the whole year after the 1929 Wall Street Crash it rose by 1.0 million.